By April 2025, there were 270 active drug shortages in the U.S.-and nearly all of them were generic medications. These aren’t rare glitches. They’re systemic failures that hit hospitals, pharmacies, and patients every single day. You might not hear about them in the news, but if you or someone you know takes insulin, vancomycin, or even a simple IV saline solution, you’ve likely felt the impact. Generic drugs make up 90% of all prescriptions filled in the U.S., yet they account for more than 70% of all shortages. Why? And what does it mean for your health?
Why Generic Drugs Are the Most Vulnerable
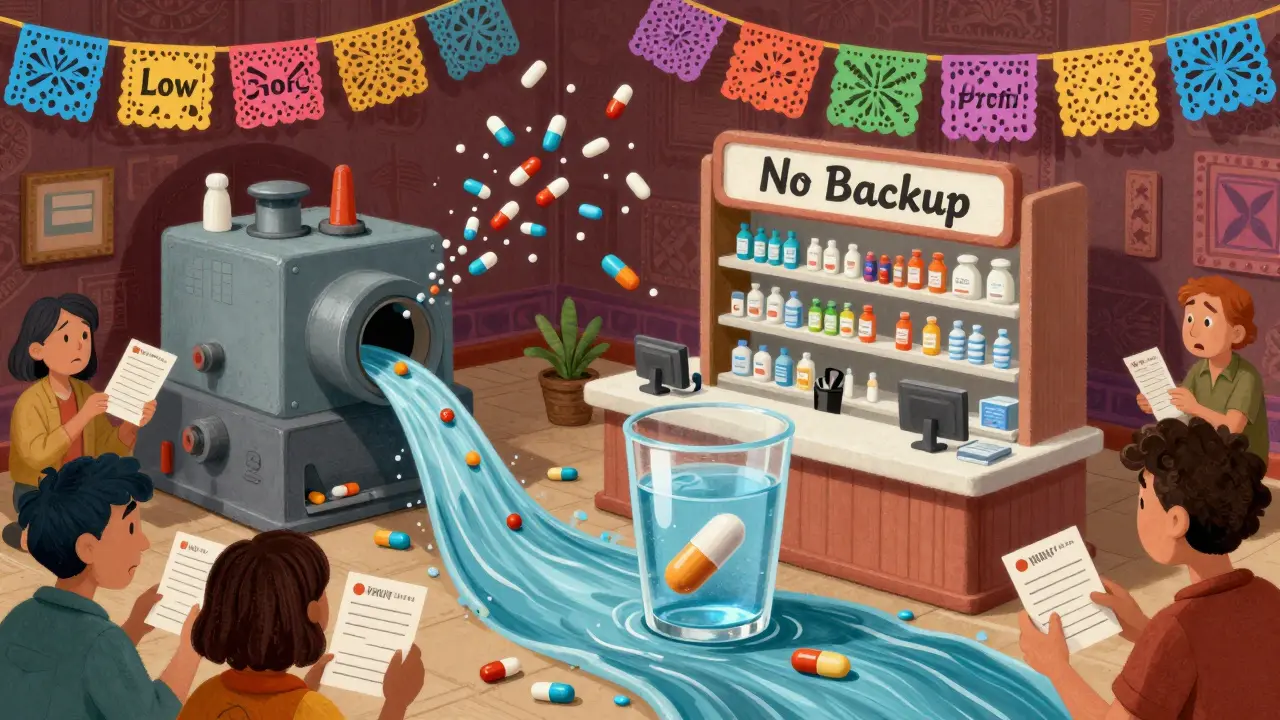
Generic drugs aren’t just cheaper versions of brand-name pills-they’re often made with razor-thin profit margins. While brand-name drugs can earn 30-40% gross margins, many generics barely scrape by at 5-10%. That’s not enough to cover the cost of modern manufacturing, quality checks, or equipment upgrades. So when a machine breaks down or a batch fails inspection, manufacturers don’t have the buffer to fix it quickly. They just stop making it.
And it’s not just about money. About 70% of generic drugs have only one or two FDA-approved manufacturers. If one plant shuts down-because of a power outage, a regulatory citation, or a supply chain hiccup-the entire country runs out. This isn’t hypothetical. In 2024, a single facility in India halted production of sterile injectables, triggering shortages of critical antibiotics like vancomycin and ampicillin across the U.S. for over eight months.
The Global Supply Chain Is a Single Point of Failure
Over 80% of the active ingredients in U.S. drugs come from just two countries: China and India. These facilities are often far from U.S. regulators, making inspections harder and delays longer. When the FDA finds a quality issue-like contaminated vials or improper sterilization-it can shut down a plant for months. And because there’s no backup supplier, the shortage hits hard.
Even basic things like IV saline bags are affected. A 2023 shortage of saline solution forced hospitals to ration fluids for emergency rooms, surgeries, and chemotherapy patients. Some nurses had to reuse bags or dilute them further, increasing the risk of infection and treatment failure. This isn’t just inconvenient-it’s dangerous.
Injectables Are the Weakest Link
More than 60% of all generic drug shortages involve sterile injectables-drugs given by injection or IV. These aren’t pills you can swallow. They’re life-saving medications like chemotherapy agents, antibiotics, and anesthetics. Making them requires clean rooms, precise temperatures, and highly trained staff. One tiny mistake can ruin an entire batch.
And there’s little room for error. A single production line for a generic injectable might cost $50 million to build and maintain. With profit margins so low, few companies are willing to invest in multiple lines. So if one line fails, there’s no backup. That’s why cancer centers reported in 2024 that 67% of them had to change chemotherapy regimens because cisplatin or doxorubicin was unavailable. Patients didn’t get the best treatment-they got whatever was left.
Shortages Don’t Just Disappear-They Get Worse
Back in 2011, the average generic drug shortage lasted about 12 months. By 2023, that number had doubled to 24 months. Why? Because the system isn’t designed to fix itself. Companies don’t get rewarded for reliability-they get rewarded for the lowest bid. Hospitals and insurers keep choosing the cheapest option, even if it’s made by a single plant with a history of quality issues.
And when a drug runs out, the price doesn’t stay low. In fact, the median price of a generic drug in shortage jumped 14.6%. Meanwhile, substitute drugs-often more expensive or less effective-can spike by three times that rate. A patient who used to pay $2 for a generic antibiotic might end up paying $60 for a different one, or worse, go without.
What Happens When You Can’t Get Your Medicine
It’s not just about delays. It’s about risk. A 2022 survey by the American Medical Association found that 63% of pharmacists reported drug shortages led to serious patient harm. That includes infections from improper substitutions, kidney failure from delayed dialysis meds, and even deaths from untreated seizures or heart conditions.
One hospital pharmacist in Ohio told a reporter in early 2025: “We had a 72-year-old man with sepsis. We couldn’t get meropenem. We used an alternative-less effective, more toxic. He spent 18 days in the ICU instead of five.”
For chronic conditions, it’s even worse. Patients with pain, epilepsy, or mental health disorders often rely on specific generics. When those disappear, doctors have to guess. A patient on a stable dose of generic carbamazepine might be switched to a different brand with different absorption rates. Seizures return. Depression worsens. Side effects flare up. No one’s to blame-but someone always pays the price.
Healthcare Workers Are Overwhelmed
Managing shortages isn’t a quick fix. It’s a full-time job. Pharmacists now spend 15-20 hours a week just tracking down alternatives, updating electronic records, and training staff. In 2025, 72% of hospitals said drug shortages made their existing staffing shortages worse. Nurses are being asked to handle more complex meds. Pharmacists are working weekends. Pharmacy techs are calling suppliers at 6 a.m. because the morning shipment didn’t arrive.
Independent pharmacies are hit hardest. According to the National Community Pharmacists Association, 78% of small pharmacies spent an average of 12.3 hours per week just finding drugs. And 43% said patients walked out because they couldn’t afford the substitute or just gave up.
Why the Market Isn’t Fixing Itself
The generic drug market used to have hundreds of manufacturers. Now, the top 10 control 60% of the business. The number of U.S.-based manufacturing facilities has dropped 22% since 2015. Why? Because it’s not profitable to make cheap drugs with high risk. The FDA has issued more quality citations than ever-but fines don’t fix broken supply chains. And when the FDA asks manufacturers to ramp up production, they say they can’t-they don’t have the capacity.
Even policy efforts have had mixed results. The 2020 Executive Order that created the Essential Medicines List helped reduce shortages of critical drugs by 32% between 2020 and 2023. But by 2024, shortages started climbing again. Why? Because the root problem-low prices, no incentives for quality, and zero backup supply-wasn’t addressed.

What Could Actually Help
Experts agree: the system needs to change. The FDA’s 2024 Drug Shortage Task Force outlined four real solutions:
- Diversify manufacturing-don’t rely on just two countries or two plants.
- Create financial incentives-pay manufacturers more for reliable, high-quality production, not just the lowest bid.
- Adopt advanced manufacturing-use newer technologies that can produce drugs faster and with fewer errors.
- Build early warning systems-track inventory and supplier risks before a shortage hits.
Some states are trying. New York and California now require hospitals to report shortages in real time. The federal government is testing pilot programs that pay manufacturers to keep extra stock of critical drugs. But without a national policy that rewards reliability over price, these efforts won’t be enough.
What You Can Do
As a patient, you can’t fix the system. But you can protect yourself:
- Ask your doctor or pharmacist: “Is this drug in short supply? Are there alternatives?”
- Don’t wait until your prescription runs out-call for refills early.
- If your medication changes, ask why-and if it’s safe.
- Report problems to your local pharmacy or hospital. Your voice matters.
And if you’re a caregiver or advocate, push for policy changes. Contact your representatives. Ask why we still allow a system where life-saving drugs vanish because no one made enough profit to keep them in stock.
Generic drugs were meant to make healthcare affordable. But when they disappear, affordability means nothing. Access does.
Why are generic drug shortages getting worse?
Generic drug shortages are worsening because manufacturers earn very little profit on these drugs-often just 5-10%-which doesn’t cover the cost of reliable production. Many have only one or two suppliers, and over 80% of active ingredients come from just two countries. When one plant shuts down due to quality issues, supply chains break. There’s no financial incentive to build backup capacity, so shortages last longer-now averaging 24 months, up from 12 in 2011.
Are brand-name drugs also in short supply?
Yes, but far less often. Brand-name drugs have higher profit margins, so manufacturers can afford to maintain extra inventory and invest in multiple production sites. While the number of brand-name drug shortages increased by 37% from 2020 to 2023, they still make up less than 30% of total shortages. More importantly, brand-name drugs often have therapeutic alternatives, while generics rarely do-making their shortages more dangerous.
What types of drugs are most likely to be in short supply?
Sterile injectables are the most vulnerable-making up about 60% of all shortages. These include antibiotics like vancomycin, chemotherapy drugs like cisplatin, anesthetics, and IV fluids like saline. They require complex, expensive manufacturing under strict sterile conditions. Even small production errors can lead to recalls, and because they’re often made by only one or two facilities, shortages spread quickly.
Do drug shortages affect patient safety?
Absolutely. A 2022 survey found that 63% of pharmacists reported drug shortages led to serious patient harm, including infections, treatment delays, and even deaths. When a drug isn’t available, doctors must use substitutes that may be less effective, more toxic, or require different dosing. Cancer patients, ICU patients, and those with chronic conditions are at highest risk.
Can I get my generic drug from another country?
Legally, no. The FDA only approves drugs manufactured in facilities it has inspected and certified. Even if you find the same generic drug sold online from India or Canada, it’s not guaranteed to be safe or identical. Importing unapproved drugs is illegal and risky-many contain incorrect doses or contaminants. Your safest option is to work with your pharmacist to find an FDA-approved alternative.
What’s being done to fix this?
The FDA is pushing for four key changes: diversifying manufacturing locations, offering financial incentives for reliable production, using advanced manufacturing tech, and creating early warning systems. Some states now require hospitals to report shortages in real time. But without a national policy that pays manufacturers for quality-not just low prices-these efforts won’t be enough to stop the trend.
What’s Next
The Congressional Budget Office predicts drug shortages will hit 350 by the end of 2026 unless something changes. Without fixing the pricing model that punishes reliability, the cycle will keep repeating: drug disappears → patients suffer → doctors scramble → manufacturers lose money → drug stays gone.
This isn’t just a pharmacy problem. It’s a public health crisis. And it’s one we can’t afford to ignore any longer.


Comments (11)
Thomas Anderson
This is insane. I had to wait three weeks for my dad’s vancomycin last year. The pharmacy called every day. No one could help. He got sicker while we played phone tag with distributors. It’s not a glitch-it’s a system designed to fail.
Sinéad Griffin
USA needs to stop outsourcing everything to India and China. We used to make our own meds. Now we’re begging for IV bags like we’re in a third-world country. 🇺🇸💊
Daniel Wevik
The structural incentives are misaligned. Generic manufacturers operate under a lowest-bidder procurement model that disincentivizes capital investment in redundant capacity, quality assurance infrastructure, and supply chain resilience. The FDA’s enforcement actions, while necessary, are reactive rather than predictive. Without risk-adjusted pricing or strategic stockpiling via public-private partnerships, we’re merely rearranging deck chairs on the Titanic.
Dwayne hiers
Let’s be clear: sterile injectables are the Achilles’ heel. The GMP requirements for aseptic filling lines are brutal-clean rooms, environmental monitoring, endotoxin testing, sterility assurance levels. A single contamination event can shut down a $50M line for 6–12 months. And with only one or two suppliers per product? That’s not a supply chain. That’s a single point of failure with a death sentence attached.
Sarthak Jain
from india here… we make a lot of these generics but the quality control is hit or miss. us agencies dont inspect often enough. and when they do, plants shut down for months. but honestly, if us paid a bit more, we could upgrade. its not about cheating, its about survival.
Alexis Wright
Oh wow, look at this. A 12-page manifesto on why capitalism failed healthcare. Let me guess-someone’s uncle died because he couldn’t get saline. Newsflash: if you want quality, pay for it. Stop pretending you want cheap drugs and then act shocked when they vanish. The market isn’t broken. You just don’t like the price tag. Welcome to reality.
Edward Stevens
So we’re supposed to be grateful that our chemotherapy drug is available… at triple the price and with a different side effect profile? Thanks for the upgrade, free market. I’ll take the original $2 generic, please. Even if it means waiting 6 months.
Jonny Moran
For anyone reading this and thinking ‘this doesn’t affect me’-it will. One day, you or someone you love will need a drug that’s no longer made. And then you’ll understand why this isn’t just about profit margins. It’s about dignity. It’s about not having to beg for your life.
jeremy carroll
my mom’s epilepsy med disappeared last year. they switched her to a different brand and she had 3 seizures in a week. the dr said ‘it’s the same thing’ but it wasn’t. i called 12 pharmacies. nobody had it. we had to drive 90 miles to get a special order. this isn’t healthcare. it’s russian roulette.
Tim Bartik
THEY’RE STEALING OUR MEDS. CHINA AND INDIA ARE HOLDING OUR LIVES HOSTAGE. WE NEED A NATIONAL DRUG MANUFACTURING CORPS. BUILD FACTORIES. PAY PEOPLE TO MAKE STERILE BAGS. THIS IS A WAR. AND WE’RE LOSING BECAUSE WE’RE TOO POLITE.
Daniel Thompson
While the systemic failures are well-documented, one overlooked variable is the role of pharmacy benefit managers (PBMs) in suppressing generic drug reimbursement rates. Their opaque rebate structures incentivize manufacturers to compete on price rather than reliability, effectively creating a race to the bottom. The FDA can regulate quality, but unless PBMs are held accountable for their role in pricing distortion, the root cause remains untouched.