Rifampin Birth Control Risk Timeline
Your Birth Control Risk Timeline with Rifampin
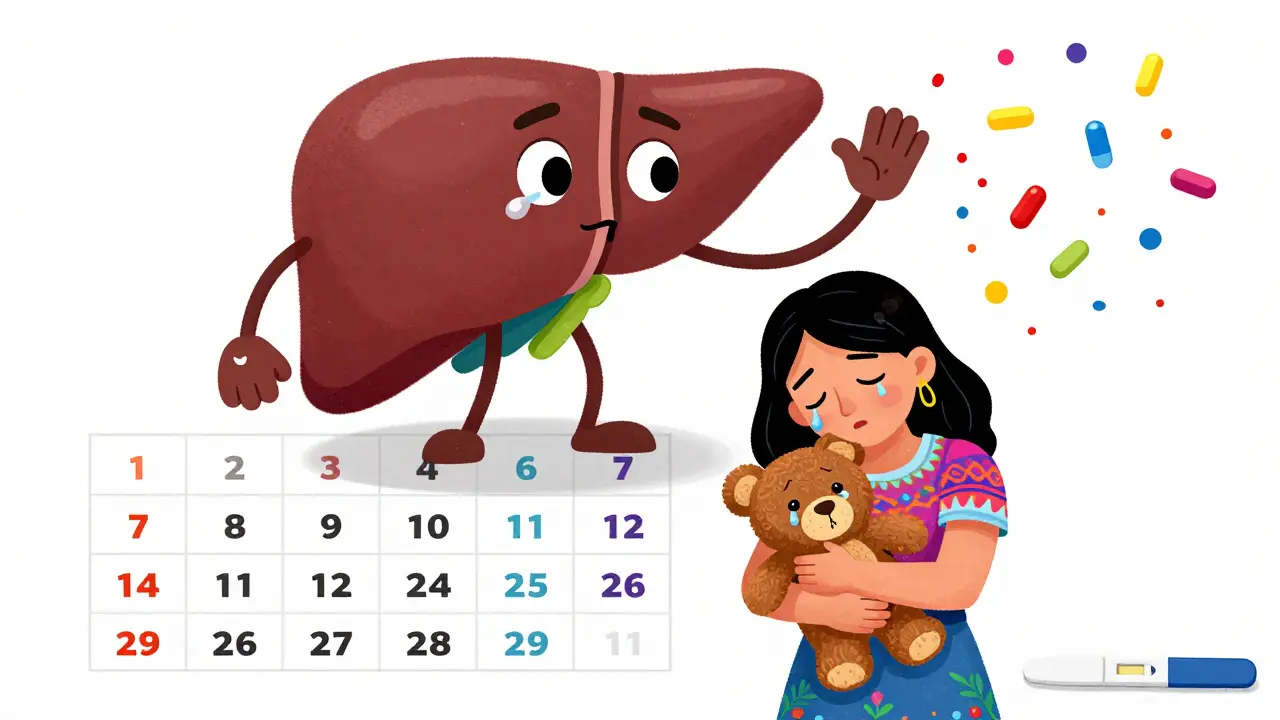
Rifampin significantly reduces the effectiveness of hormonal birth control. This timeline shows when your birth control is at risk and when you need backup contraception.
• Estrogen down by up to 67% • Progestin down by up to 50% Very high risk of pregnancy.
but enzyme induction continues for 2-4 weeks. High risk remains for 28 days.
Birth control methods return to full effectiveness.
No risk from rifampin interaction.
What You Must Do
- Copper IUD (best option)
- Condoms with spermicide
- Permanent contraception (tubal ligation or vasectomy)
- Birth control pill
- Birth control patch
- Birth control ring
- Birth control shot
- Implants (Nexplanon)
These will NOT protect you due to rifampin's enzyme-inducing effect.
When you're taking rifampin for tuberculosis or a stubborn staph infection, the last thing you want to worry about is accidentally getting pregnant. But here’s the hard truth: rifampin can make your birth control pill useless - and most people have no idea.
This isn’t a theory. It’s been documented since the 1970s. Women on the pill who took rifampin for TB have gotten pregnant - even when they took their pill every single day. No missed doses. No vomiting. Just rifampin doing its job too well.
Rifampin doesn’t just kill bacteria. It also wakes up your liver enzymes like a drill sergeant. Specifically, it turns on CYP3A4, the enzyme that breaks down hormones. And that includes the estrogen and progestin in your birth control. Within 24 to 48 hours of starting rifampin, your body starts flushing those hormones out faster than your pill can replace them. Studies show estrogen levels can drop by up to 67%. Progestin levels? Down by half. That’s not a small tweak. That’s a full system override.
Why Rifampin Is the Only Antibiotic That Really Matters
You’ve probably heard warnings about antibiotics and birth control. Maybe your doctor told you to use condoms while on antibiotics. That advice? Mostly wrong.
Penicillin? Tetracycline? Azithromycin? Erythromycin? None of them reliably interfere with hormonal birth control. A 2018 review in BJOG looked at every study ever done on this. Only one antibiotic consistently caused contraceptive failure: rifampin.
There were 117 reports in the UK between 1970 and 1999 linking other antibiotics to pregnancy. But when researchers tested those cases in controlled studies? No increase in ovulation. No drop in hormone levels. Just bad luck and coincidence. Rifampin is the only one that actually changes how your body handles hormones.
Even rifabutin - a cousin of rifampin used for HIV-related infections - is less risky. At 300mg daily, it cuts hormone levels by about 20-30%. Rifampin at 600mg? 50% or more. That’s the difference between a warning and a red flag.
How Long the Risk Lasts (And Why It’s Longer Than You Think)
Some people think, “I’m done with rifampin after two weeks - my birth control should be fine.” Wrong.
Rifampin’s effect on liver enzymes doesn’t vanish when you stop taking it. The enzymes stick around. Your liver keeps churning out those hormone-busting enzymes for weeks. That’s why experts say you need backup contraception for 28 days after your last dose.
Even though rifampin leaves your blood in 3 to 4 hours, the enzyme induction lasts 2 to 4 weeks. That’s not a guess. It’s based on pharmacokinetic studies tracking hormone levels and ovulation markers. If you go off rifampin and start relying on the pill again after just 7 days? You’re gambling with pregnancy.
And here’s the scary part: no one’s ever done a study that directly counted how many women got pregnant while on rifampin. We don’t have exact numbers. We only know what happens to hormone levels and ovulation. But we know enough to say: if your hormones are cut in half, you’re not protected.

What Backup Contraception Actually Works
So what do you use instead? Not another pill. Not the patch. Not the ring. Those all rely on hormones - and rifampin will break them too.
The only safe options are non-hormonal methods:
- Copper IUD - No hormones. Works for up to 12 years. The gold standard for women on rifampin.
- Condoms - Not ideal alone, but better than nothing. Use with spermicide if you can.
- Permanent options - Tubal ligation or vasectomy for partners if you’re done having kids.
What about implants like Nexplanon? A small 2023 study followed 47 women using etonogestrel implants while on rifampin. Zero pregnancies. That’s promising. But it’s still a tiny sample. Until more data comes in, the official advice remains: avoid all hormonal methods.
The CDC says combined hormonal contraceptives (the pill, patch, ring) are Category 4 with rifampin - meaning the risks outweigh any benefits. That’s the highest warning level. Don’t ignore it.
Why Doctors Still Get This Wrong
Here’s the broken part: most doctors don’t talk about this.
A 2017 survey found only 42% of primary care doctors consistently warn patients about rifampin and birth control. Twenty-eight percent tell everyone to use condoms with any antibiotic. That’s not helpful. It’s noise.
And when patients do get warned? Often too late. Many are prescribed rifampin for TB, get the pill refill, and only find out about the interaction after they miss a period. A 2022 study in Journal of Women’s Health found 63% of women on rifampin got inadequate counseling.
Part of the problem? It’s not taught well. Medical schools still lump all antibiotics together. But rifampin isn’t like amoxicillin. It’s a metabolic powerhouse. And if you’re a woman of childbearing age, that matters.
What’s Changing in Treatment and Research
Thankfully, things are shifting.
The WHO now recommends copper IUDs or implants as first-line birth control for women needing rifampin-based TB treatment. In places like sub-Saharan Africa, where TB is common and access to contraception is limited, this guidance is life-changing.
Drug makers are also adapting. New birth control pills now have to be tested against rifampin before they’re approved. The FDA and EMA require it. That’s why newer pills often come with stronger warnings - and why some are designed to be more resistant to enzyme induction.
There’s also hope in new TB regimens. A 4-month treatment using rifapentine and moxifloxacin (instead of rifampin) is being tested. Early results look good. If approved, it could replace rifampin in many cases - removing the contraceptive risk entirely.
But until then? Rifampin is still the go-to for TB. And if you’re on it, your birth control pill isn’t enough.
What You Should Do Right Now
If you’re prescribed rifampin:
- Ask your doctor: “Is this going to affect my birth control?” Don’t assume they know.
- Get a copper IUD inserted before you start rifampin - it’s the most reliable option.
- If you can’t get an IUD, use condoms with every sexual encounter - no exceptions.
- Keep using backup contraception for 28 days after your last rifampin dose.
- Don’t switch to another pill, patch, or ring. They won’t work.
If you’re already on rifampin and didn’t know about this interaction:
- Use condoms immediately - even if you’re in the middle of your pill pack.
- Take a pregnancy test if your period is late or you feel off.
- Schedule an appointment to discuss long-term contraception options.
This isn’t about being paranoid. It’s about being informed. Rifampin saves lives. But it can also change your future if you don’t plan for it.
Does rifampin make birth control pills completely useless?
Yes. Rifampin significantly reduces hormone levels from birth control pills - by up to 67% for estrogen and over 50% for progestin. This drops hormone concentrations below the level needed to prevent ovulation. Even perfect pill use won’t protect you.
What about other antibiotics like amoxicillin or azithromycin?
No evidence shows they interfere with birth control. While there were old reports linking penicillin and tetracycline to pregnancy, controlled studies found no drop in hormone levels or increase in ovulation. Only rifampin and possibly rifabutin have proven effects.
How long should I use backup contraception after stopping rifampin?
For 28 days after your last dose. Rifampin keeps inducing liver enzymes for weeks after you stop taking it. Stopping backup too soon puts you at risk of pregnancy, even if you’ve finished your antibiotic course.
Can I switch to a different birth control method while on rifampin?
Only non-hormonal methods are safe: copper IUD or condoms. Hormonal methods - including the implant, patch, ring, or shot - are not reliable with rifampin. Even the implant, while promising in small studies, hasn’t been proven safe enough to recommend without more data.
Is there a birth control pill that works with rifampin?
No. No currently available oral contraceptive has been shown to remain effective during rifampin use. Manufacturers test new pills against rifampin, but so far, none have passed. The only solution is non-hormonal backup.
Why don’t more doctors warn patients about this?
Many doctors still believe all antibiotics affect birth control, which isn’t true. Others assume patients already know. A 2017 survey found only 42% of primary care providers consistently counsel patients on this interaction. It’s a gap in education - not a lack of evidence.
Can I use emergency contraception if I had unprotected sex while on rifampin?
Yes - but not the pill form. Levonorgestrel emergency contraception (like Plan B) is metabolized by the same liver enzymes and may be less effective. The best option is a copper IUD, which works as emergency contraception and provides ongoing protection. If you can’t get an IUD, ulipristal acetate (Ella) is more reliable than levonorgestrel, but still not ideal with rifampin.


Comments (13)
Henry Ip
This is one of those posts that should be mandatory reading for every woman on birth control. I never knew rifampin was this dangerous. I thought all antibiotics were the same. Thanks for laying it out so clearly.
Just got prescribed rifampin for TB last week. I’m scheduling my IUD insertion tomorrow.
Kasey Summerer
So let me get this straight... the one antibiotic that actually breaks your pill is also the one that saves your life from TB? 🤡
Thanks, medicine. You're a real sweetheart.
kanchan tiwari
I can't believe this isn't on every pill bottle. This is a MASSIVE cover-up. Big Pharma doesn't want you to know how easily your hormones can be wiped out. They'd rather you get pregnant and then sell you a new pill. It's evil. I'm telling everyone I know.
Bobbi-Marie Nova
I’m so mad I didn’t know this. I took rifampin for a year and just assumed my pill was fine. I’m lucky I didn’t get pregnant. Now I’m scared to even look at my birth control again.
Also, why is the copper IUD so hard to get? My doctor acted like I was asking for a spaceship.
Allen Davidson
Stop treating this like it’s a mystery. It’s not. The science is clear. Rifampin induces CYP3A4. Hormones get metabolized. End of story.
Doctors who don’t know this aren’t just negligent-they’re dangerous. If you’re on rifampin and still using the pill, you’re playing Russian roulette with your fertility.
Rob Deneke
I had TB last year and took rifampin for 6 months. My doc told me to use condoms but didn’t say why. I thought it was just being extra. Turns out he was right but didn’t explain it at all. This post explains everything I should’ve known. Thank you
Riya Katyal
Oh so now you're telling me I've been using birth control wrong this whole time? And my doctor never told me? Typical. You know what they say - if you want the truth, Google it yourself.
waneta rozwan
I'm so tired of women acting like they're the only ones who have to worry about this. Men get antibiotics too. Why aren't we talking about how rifampin affects their testosterone? Oh right - because no one cares about men's health unless it's a prostate issue.
Also, why is everyone so shocked? This has been known since the 70s. You just didn't want to believe it.
Nicholas Gabriel
I’m so glad this is getting attention. I’m a nurse, and I’ve seen too many women come in with unexpected pregnancies after rifampin. One woman cried because she thought her pill was enough - she’d been taking it religiously for 5 years. The fact that this isn’t standard counseling is heartbreaking.
Please, if you’re on rifampin: get the IUD. Don’t wait. Don’t hope. Don’t assume. Just do it.
swarnima singh
this is why i stopped trusting doctors. they all just parrot what they read in some outdated textbook. no one ever tells you the real truth. the system is rigged. the pill was never meant to be safe. it was meant to make you dependent. and now they want you to pay for an iud too? capitalism is evil.
Isabella Reid
I’m from India and we don’t have easy access to IUDs here. My doctor just told me to use condoms. I did. But I also started tracking my cycle like a hawk. It’s not ideal, but it’s what I’ve got. Thanks for the info - I’ll share it with my friends.
Jody Fahrenkrug
I’m so glad someone finally said this. I had a friend who got pregnant on rifampin and thought she was ‘bad at birth control.’ She wasn’t. She was just unlucky with the meds. This needs to be common knowledge.
john Mccoskey
Let’s be brutally honest here. The entire medical establishment is built on layers of misinformation, passive negligence, and profit-driven inertia. Rifampin’s interaction with hormonal contraceptives is not a ‘gap in education’ - it’s a systemic failure. Medical schools still teach antibiotics as a monolithic category because it’s easier than teaching pharmacokinetics. Pharmaceutical companies don’t fund studies on non-hormonal alternatives because they don’t make money off them. The CDC’s Category 4 warning is a legal shield, not a safety net. And women? Women are the collateral damage in a system that treats their reproductive health as an afterthought. You want to fix this? Stop asking doctors. Start demanding policy change. Stop trusting institutions. Start demanding transparency. And if you’re on rifampin right now? Stop reading Reddit. Go get an IUD. Now.