Gabapentin Safety: What You Need to Know About Side Effects, Risks, and Proper Use
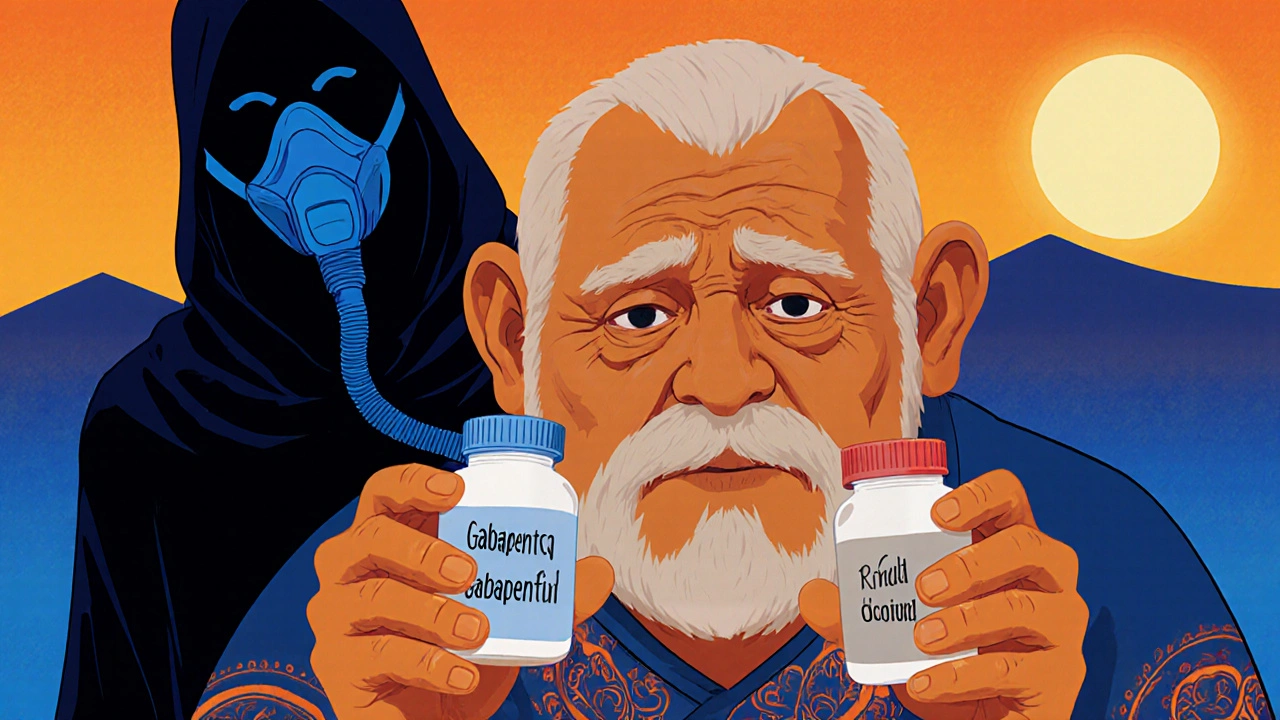
When you take gabapentin, a prescription nerve pain and seizure medication often used for neuropathic pain and restless legs. Also known as Neurontin, it works by calming overactive nerves in your brain and spinal cord. But gabapentin isn’t harmless—especially if you don’t use it right. People take it for back pain, anxiety, or insomnia, but many don’t realize how easily it can cause dizziness, swelling, or worse when mixed with other drugs. The FDA has warned about serious breathing problems when gabapentin is taken with opioids or sedatives, and these risks go up if you’re older or have lung issues.
Another big concern is gabapentin withdrawal, the uncomfortable and sometimes dangerous symptoms that happen when you stop taking it too fast. Unlike some meds, you can’t just quit gabapentin cold turkey. People report seizures, panic attacks, sweating, and insomnia if they stop abruptly—even after just a few weeks. That’s why doctors tell you to taper off slowly, like you would with benzodiazepines. And don’t assume it’s safe just because it’s not an opioid. It affects the same brain pathways, and misuse is rising, especially among people who combine it with alcohol or painkillers. Then there’s gabapentin dosage, the amount you take that makes the difference between relief and risk. The typical starting dose is 300 mg once a day, but some people end up on 3,600 mg daily. Higher doses don’t always mean better pain control—they just raise your chance of drowsiness, blurred vision, or loss of coordination. If you’re over 65, your kidneys process it slower, so your doctor should lower your dose. And if you’re taking it with blood pressure medications, like calcium channel blockers or ACE inhibitors, you might get extra dizziness or low blood pressure, which increases fall risk.
You’ll also see gabapentin mentioned alongside other drugs in our posts—like how antihistamines and alcohol can worsen drowsiness, and gabapentin does the same. Mixing it with anything that slows your brain down—sleep aids, muscle relaxants, even some cold medicines—can be risky. That’s why lab monitoring calendars are useful for people on multiple meds. You need to track not just how you feel, but your kidney function too, since gabapentin leaves your body through your kidneys. If you’re on dialysis or have chronic kidney disease, your dose must be adjusted.
What you won’t find in most ads is that gabapentin isn’t always the best choice. For nerve pain, other options like pregabalin or certain antidepressants may work better with fewer side effects. And if you’re taking it for anxiety or sleep without a diagnosis, you’re using it off-label—and that’s where misuse starts. The goal isn’t just to take it, but to take it safely. That means knowing your dose, avoiding dangerous combos, and never stopping without help.
Below, you’ll find real-world advice from people who’ve managed gabapentin use, stopped it safely, or dealt with side effects. No fluff. Just what works—and what to avoid.