Gastric Cancer: What You Need to Know Right Now
If you’ve heard the term “gastric cancer” and feel confused, you’re not alone. It’s simply a type of cancer that starts in the lining of your stomach. Knowing the basics can help you spot warning signs early and understand what doctors will do if they find it.
What Triggers Stomach Cancer?
The biggest risk factor is infection with Helicobacter pylori (H. pylori). This bacteria lives in the stomach lining and can cause ulcers that, over years, may turn cancerous. Other common triggers include a diet high in salty or smoked foods, smoking cigarettes, heavy alcohol use, and a family history of gastric tumors.
Age matters too – most cases show up after 50. If you’ve had long‑term stomach inflammation, such as chronic gastritis or intestinal metaplasia, your risk goes up. Certain genetic conditions, like hereditary diffuse gastric cancer (HDGC), also raise the odds, even in younger people.
It’s worth checking if you have any of these factors. A simple breath test or stool sample can spot H. pylori, and doctors can treat it with antibiotics before problems develop.
How Is It Treated?
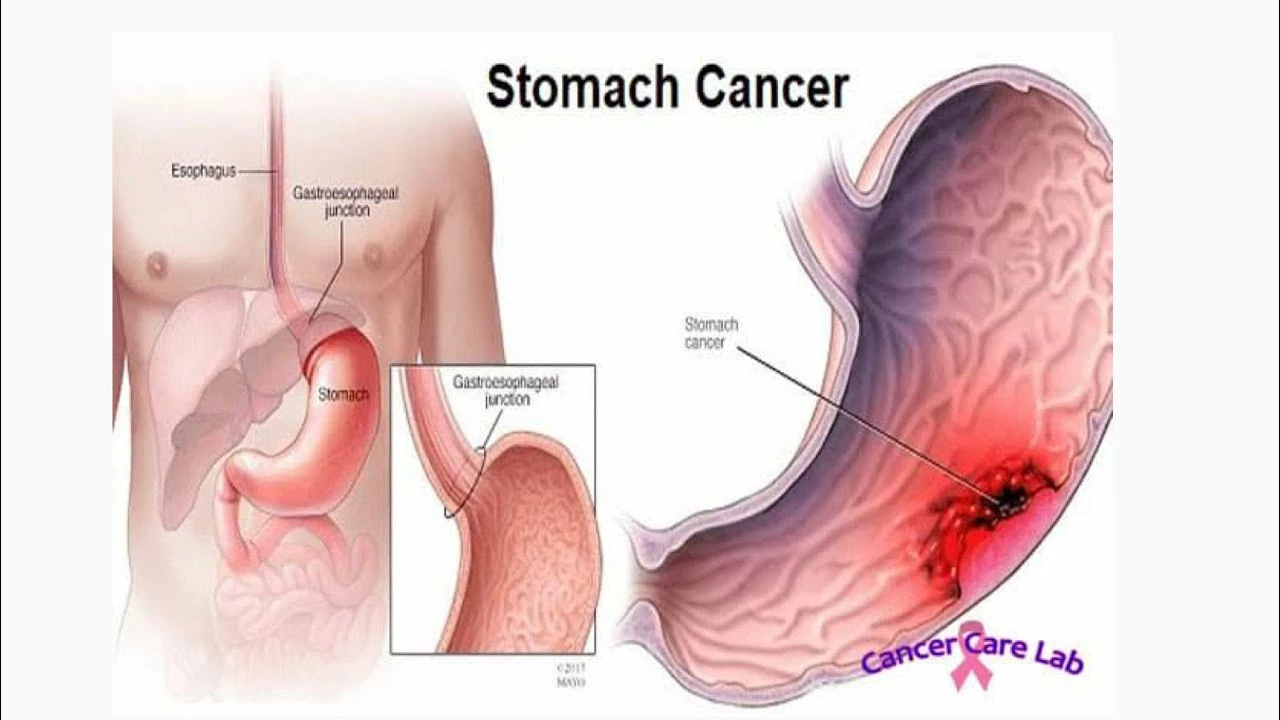
When a doctor suspects gastric cancer, they’ll order an endoscopy – a thin tube with a camera that lets them see the stomach lining and take a biopsy. If the lab confirms cancer, treatment plans usually combine surgery, chemotherapy, and sometimes radiation.
Surgery is often the first step if the tumor hasn’t spread far. Surgeons may remove part of the stomach (partial gastrectomy) or the whole organ (total gastrectomy), plus nearby lymph nodes to check for spread.
Chemotherapy can be given before surgery (neoadjuvant) to shrink the tumor, or after surgery (adjuvant) to kill leftover cells. Common drug combos include fluorouracil with oxaliplatin or capecitabine with cisplatin. Your oncologist will pick what fits your health and cancer stage.
In some cases, targeted therapy like trastuzumab is added if the tumor tests positive for HER2 protein. Newer immunotherapy drugs such as pembrolizumab are also showing promise, especially for advanced disease.
If surgery isn’t an option because the cancer has spread widely, doctors focus on systemic treatments (chemo and targeted drugs) to control growth and relieve symptoms.
Living with gastric cancer means staying in touch with your care team. Nutritional support is crucial – after stomach surgery you’ll need smaller, more frequent meals and possibly vitamin supplements. Join a support group or talk to a dietitian; they can help you keep weight and energy up.
Bottom line: early detection saves lives. If you have persistent indigestion, unexplained weight loss, vomiting blood, or notice your stomach feels full after tiny bites, call a doctor right away. Simple tests can catch problems before they turn serious.
At CanDrug Pharma Knowledge Hub we keep the info clear and up‑to‑date so you can make confident health choices. Bookmark this page, share it with friends who might need it, and remember: knowing the facts is the first step toward staying healthy.