Sjogren’s syndrome is a chronic autoimmune disease that primarily targets the body’s exocrine glands, leading to dry eyes and dry mouth. When the glands that moisten the urinary tract are compromised, infections can become more frequent.
Understanding Sjogren’s Syndrome
Sjogren’s syndrome affects about 4million adults in the United States, with women making up 90% of cases. The disease is characterized by the presence of auto‑antibodies such as SSA/Ro and SSB/La, and it is diagnosed using the American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) criteria, which include a salivary gland biopsy.
The hallmark symptoms-xerostomia (dry mouth) and xerophthalmia (dry eyes)-are easy to spot, but many patients also experience systemic issues like joint pain, fatigue, and importantly, urinary disturbances.
How Sjogren’s Impacts the Urinary Tract
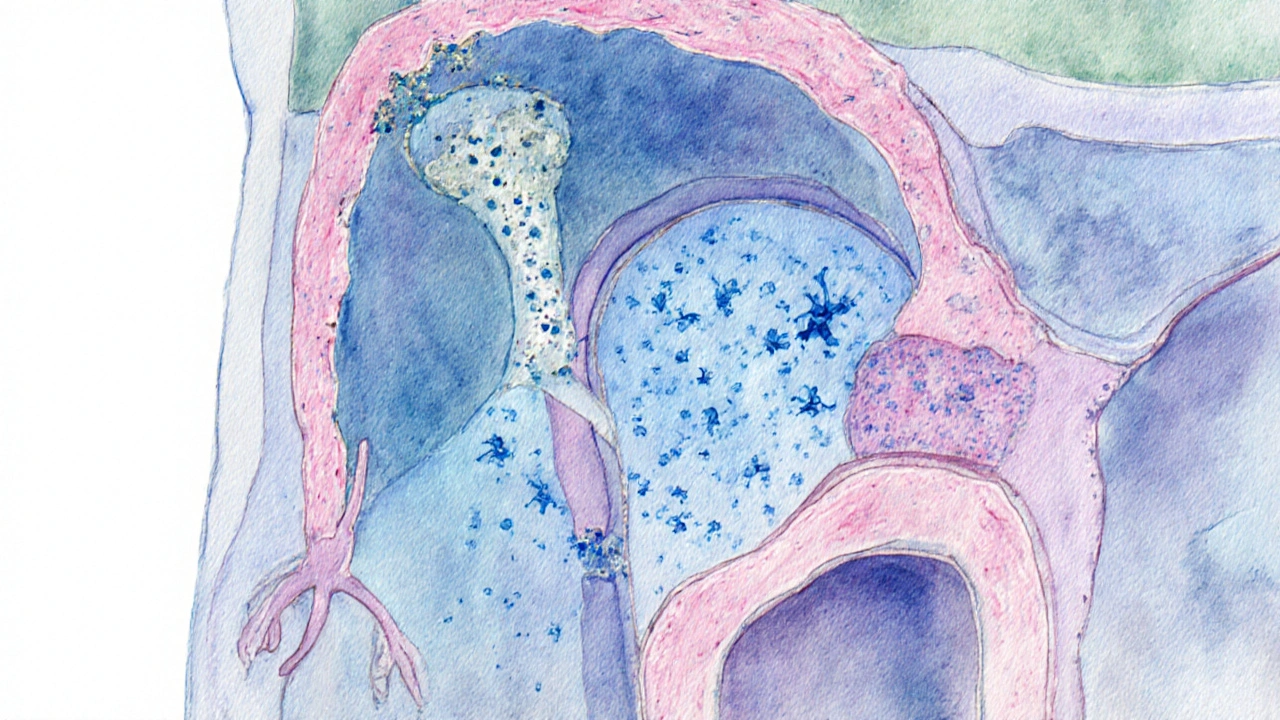
The urinary tract relies on mucus secretions from the urethral glands to maintain a protective barrier. In Sjogren’s, the same immune attack that shrinks salivary glands can reduce the output of these mucus‑producing cells, creating a dry environment that favors bacterial growth.
Other mechanisms include:
- Autonomic dysfunction: Many patients develop dysautonomia, which can impair bladder emptying and lead to residual urine-prime breeding ground for pathogens.
- Chronic inflammation: Elevated cytokines (IL‑6, TNF‑α) increase bladder wall permeability, allowing microbes to adhere more easily.
- Medication side‑effects: Drugs commonly used to manage Sjogren’s (e.g., antihistamines for dry eyes) may further reduce urinary flow.
UTI Patterns Seen in Sjogren’s Patients
Studies from Australian rheumatology centres report that up to 30% of Sjogren’s patients experience recurrent urinary tract infections (rUTIs), compared with 8% in the general population. The typical pathogens remain Escherichia coli and Klebsiella pneumoniae, but there’s a higher incidence of Enterococcus faecalis, which thrives in low‑moisture environments.
Key clinical clues include:
- Frequent dysuria without classic pyuria on dipstick.
- Positive urine culture despite low symptom severity.
- Concurrent symptoms of dryness in other mucosal sites.
UTI vs. Interstitial Cystitis: A Quick Comparison
| Attribute | Urinary Tract Infection | Interstitial Cystitis |
|---|---|---|
| Typical Symptom | Burning during urination, urgency | Chronic pelvic pain, urgency without infection |
| Urine Culture | Positive (>10⁵ CFU/mL) | Negative |
| Primary Trigger | Bacterial colonisation | Bladder lining dysfunction |
| Relation to Sjogren’s | Higher incidence due to glandular dryness | Often co‑exists; shared autonomic dysfunction |
| First‑line Treatment | Antibiotics (e.g., nitrofurantoin) | Pelvic floor therapy, bladder instillations |
Distinguishing between the two is vital; treating an interstitial cystitis flare with antibiotics offers no benefit and can foster resistance.
Diagnosing a UTI in the Context of Sjogren’s
Standard urine dipsticks may be misleading because the inflammatory milieu can mask leukocyte esterase. Clinicians should:
- Obtain a mid‑stream clean‑catch sample for culture.
- Consider C‑reactive protein (CRP) and erythrocyte sedimentation rate (ESR) to gauge systemic inflammation.
- Screen for bladder dysfunction via post‑void residual (PVR) ultrasound.
Positive SSA/Ro antibodies and a recent salivary gland biopsy (salivary gland biopsy shows focal lymphocytic sialadenitis) bolster the diagnosis of Sjogren’s‑related UTI risk.
Management Strategies
Effective care combines infection control with addressing the underlying dryness.
- Hydration: Aim for at least 2.5L of fluid daily; citrus‑based drinks may irritate dry mucosa, so opt for herbal teas or water.
- Antibiotic stewardship: Use culture‑guided agents, limit course to 5-7days to curb resistance.
- Immunomodulation: Disease‑modifying drugs such as hydroxychloroquine can reduce overall auto‑immune activity, indirectly lowering UTI frequency.
- Topical lubrification: Vaginal and urethral moisturisers (glycerin‑based) restore mucosal barrier.
- Bladder training: Timed voiding every 3hours reduces residual urine.
- Probiotics: Strains like Lactobacillus rhamnosus help maintain a healthy urogenital flora.
Patients with severe autonomic dysfunction may benefit from a low‑dose anticholinergic regimen to improve bladder emptying, but this must be balanced against the risk of worsening dry mouth.
Related Concepts and Wider Context
Understanding the UTI‑Sjogren’s link opens doors to other systemic connections:
- Other autoimmune diseases: Lupus, rheumatoid arthritis, and scleroderma also show elevated UTI rates due to similar glandular involvement.
- Exocrine gland dysfunction: Beyond saliva and tears, nasal and gastrointestinal mucosa can be compromised, explaining why some patients report chronic sinus infections.
- Renal involvement: Interstitial nephritis is a rare but documented complication of Sjogren’s, highlighting the need for regular kidney function monitoring.
Future research is focusing on biomarkers that predict urological complications, such as urinary cytokine panels (IL‑8, MCP‑1) and imaging of bladder wall thickness via ultrasound.
Take‑Home Checklist for Patients and Clinicians
- Ask about urinary symptoms during every Sjogren’s follow‑up.
- Maintain adequate fluid intake and consider urethral moisturisers.
- Obtain a urine culture before starting antibiotics.
- Screen for bladder emptying issues with post‑void residual testing.
- Discuss immunomodulatory therapy options with a rheumatologist.
By integrating these steps, the cycle of recurrent infections can be broken, improving quality of life for those living with Sjogren’s syndrome.

Frequently Asked Questions
Why are UTIs more common in people with Sjogren’s syndrome?
The autoimmune attack reduces mucus production in the urinary tract, creates dry mucosal surfaces, and often impairs bladder emptying. Both factors give bacteria a foothold, leading to higher infection rates.
Can I treat a UTI with over‑the‑counter pain relievers alone?
Pain relievers may ease discomfort, but they don’t eradicate the bacteria. A culture‑directed antibiotic course is essential, especially because recurrent infections are common in Sjogren’s.
How can I tell if my symptoms are a UTI or interstitial cystitis?
A positive urine culture (>10⁵CFU/mL) points to a UTI, while a negative culture with persistent pelvic pain suggests interstitial cystitis. A doctor may also measure post‑void residual volume to help differentiate.
Are there lifestyle changes that reduce UTI risk for Sjogren’s patients?
Yes. Stay well‑hydrated, use urethral moisturisers, practice timed voiding, avoid irritating soaps, and consider probiotics to maintain healthy flora.
Does hydroxychloroquine help prevent UTIs?
Hydroxychloroquine lowers overall autoimmune activity, which can indirectly reduce glandular dryness and bladder dysfunction, thereby decreasing UTI frequency. It’s not a direct antimicrobial.

Comments (16)
Destiny Hixon
These so called autoimmune excuses are just a way for pharma to push more pills
mike brown
Look, the article tries to sound scientific but it’s basically re‑hashing old textbook stuff. The link between dry glands and UTIs is obvious, yet they drown it in jargon. I’d rather see real patient data than another review.
shawn micheal
I get why this feels overwhelming for patients, but there are practical steps that really help. Staying hydrated, using gentle moisturizers, and timed voiding can cut down infection risk. Also, talking to a rheumatologist about hydroxychloroquine might address the underlying dryness. Remember, you’re not alone in navigating these challenges, and small adjustments add up. Keep pushing for the care you deserve.
Stephen Jahl
From a pathophysiological standpoint, the author delineates the mucosal desiccation cascade with reasonable accuracy, yet the exposition suffers from a paucity of quantitative metrics. The referenced cytokine milieu-principally IL‑6 and TNF‑α-warrants a deeper discussion concerning their impact on urothelial tight junction integrity. Moreover, the omission of bladder uroplakin expression data represents a notable lacuna in the mechanistic narrative. Future iterations would benefit from integrating urographic findings and correlating them with post‑void residual volumes. In sum, while the review is comprehensive in scope, it remains qualitatively descriptive rather than empirically substantiated.
Samantha Kolkowski
I see your point but the data still feels thin.
Kenneth Mendez
What they don’t tell you is that the pharma lobby funds the very studies that keep this dryness narrative alive, steering us away from cheaper natural remedies.
Gabe Crisp
Such theories oversimplify a complex autoimmune process.
Paul Bedrule
The interplay between exocrine insufficiency and microbial colonization can be viewed as a micro‑cosmic reflection of systemic dysregulation, a testament to the body’s hierarchical interdependence.
yash Soni
Oh great, another exhaustive list of things we already know, as if we needed a dissertation to realize that drinking water helps.
Emily Jozefowicz
While the sarcasm is noted, the practical checklist-hydration, moisturizers, culture‑guided antibiotics-remains solid advice for anyone managing Sjögren‑related UTIs.
Sonia Michelle
Living with Sjögren’s syndrome can feel like navigating a maze where every turn reveals a new layer of discomfort.
One of the most underappreciated aspects is how the dryness of mucosal surfaces extends beyond the eyes and mouth.
When the urethral lining loses its lubricating mucus, bacteria find an unexpected foothold.
This biological vulnerability is compounded by autonomic dysfunction that hampers complete bladder emptying.
Consequently, residual urine becomes a fertile breeding ground for pathogens such as E. coli and Enterococcus faecalis.
Patients often report subtle dysuria without the classic signs of infection, which can delay appropriate treatment.
A proactive approach involves scheduled voiding, adequate fluid intake, and the judicious use of urethral moisturizers.
Hydration alone, however, is not a panacea; the composition of the fluids matters to avoid irritating a sensitized urothelium.
Incorporating probiotics, particularly Lactobacillus strains, may help rebalance the urogenital microbiome.
From a therapeutic standpoint, culture‑directed antibiotics remain the cornerstone for acute episodes.
Yet, long‑term stewardship calls for short courses and careful monitoring to prevent resistance.
Adjunctive immunomodulation, such as hydroxychloroquine, can mitigate systemic inflammation and indirectly support glandular function.
Close collaboration between rheumatologists and urologists ensures that bladder training and post‑void residual assessments are not overlooked.
Patients should also be educated about the potential urinary side‑effects of common dry‑eye medications like antihistamines.
Mindfulness about over‑the‑counter pain relievers is crucial, as they mask symptoms without eradicating the infection.
Ultimately, a multidisciplinary plan that addresses hydration, mucosal protection, microbial control, and autoimmune activity offers the best chance to break the cycle of recurrent UTIs.
Neil Collette
Ah, the noble long‑form essay, because a 300‑word comment isn’t sufficient to convey the profundity of a simple checklist.
James Lee
Your rambling just proves the point.
Dennis Scholing
I respectfully disagree; the evidence supporting comprehensive bladder training supersedes anecdotal skepticism, and I encourage readers to consult peer‑reviewed guidelines for best practices.
Kasey Lauren
You’ve got this, keep taking those small steps!
Abhimanyu Singh Rathore
Indeed, the recommendation to “drink water” should be accompanied by a clarifying clause: ‘provided the water is at a tolerable temperature and does not contain irritants.’.