Imagine touching a light blanket and it feels like sandpaper. Or walking on a carpet that burns your feet-even though there’s no injury, no swelling, no visible damage. This isn’t imagination. It’s central sensitization. It’s when your nervous system gets stuck on high volume, turning harmless signals into intense pain. And it’s not rare. Around 2-4% of people worldwide live with this invisible, misunderstood condition every day.
What Exactly Is Central Sensitization?
Central sensitization isn’t just pain. It’s pain that’s been rewired. Your brain and spinal cord, which normally act like filters for pain signals, start misfiring. They become hypersensitive. Even tiny signals-like a breeze or a hug-get amplified into burning, stabbing, or aching pain. This happens because the nerves in your spinal cord become more excitable, the connections between them strengthen, and the body’s natural pain brakes weaken. This isn’t new. Back in 1983, neuroscientist Clifford J. Woolf first described it as the spinal cord’s "wind-up" effect. Think of it like turning up the bass on a speaker until even whispers sound like shouts. The original injury or inflammation might be long gone, but the nervous system keeps screaming. It’s not about being weak. It’s not "all in your head." It’s biology. Brain scans show 20-35% more activity in pain-processing areas. Chemicals like cytokines rise by 30-50% in affected nerves. Your body’s own painkillers-endorphins and opioids-stop working as well, with mu-opioid receptor binding dropping by 15-25%. This is measurable. It’s real. And it’s changing how we treat chronic pain.How Do You Know If You Have It?
There’s no single blood test. But there are clear signs. If your pain:- Spreads beyond the original injury site-like after a knee surgery, but now your shoulder and hip hurt too
- Feels like burning, tingling, or electric shocks without visible damage
- Gets worse from light touch, clothing, or even a gentle pat
- Is constant, even when you’re resting or sleeping
- Is out of proportion to what you’d expect from the injury
Conditions Linked to Central Sensitization
This isn’t just one condition. It’s the hidden engine behind many chronic pain disorders:- Fibromyalgia: Up to 90% of people with fibromyalgia show clear signs. That’s why they hurt all over, even without joint damage.
- Chronic low back pain: After 3 months, 35-45% of cases aren’t about discs or muscles anymore-they’re about the nervous system.
- Migraines and tension headaches: The brain’s pain circuits get stuck in overdrive, making light, sound, and smell unbearable.
- Post-surgical pain: 15-30% of people develop ongoing pain after surgery, even when the wound healed perfectly.
- Post-viral syndromes: After infections like Lyme, Epstein-Barr, or even long COVID, 65% of those with lingering pain show central sensitization markers.
Why Do Some People Develop It and Others Don’t?
It’s not random. Genetics play a role. So do past traumas-physical or emotional. Chronic stress raises cortisol and norepinephrine, which can trigger neural changes. In fact, norepinephrine levels rise 25-40% in people with this condition, keeping the nervous system on edge. Sleep loss makes it worse. Poor sleep reduces the brain’s ability to dampen pain signals. Anxiety and depression don’t cause it-but they feed it. The brain’s fear circuits and pain circuits overlap. When you’re anxious, your nervous system becomes more reactive. And here’s the cruel twist: the more you fear pain, the more your brain amplifies it. It’s a loop. Pain causes fear. Fear increases sensitivity. Increased sensitivity causes more pain. And the cycle tightens.
How Is It Treated?
Forget just popping pills. Central sensitization needs a three-pronged approach: medication, movement, and mindset. Medications:- Pregabalin (Lyrica) or gabapentin: These calm overactive nerves. 300-1200mg daily helps 55% of patients cut pain by 30-50%.
- Duloxetine (Cymbalta): An SNRI that boosts serotonin and norepinephrine. 60mg daily reduces pain by 30% in 45% of users.
- Low-dose naltrexone (LDN): 4.5mg at night. Surprisingly, this opioid blocker reduces inflammation in the brain and helps 40% of fibromyalgia patients.
- Nortriptyline: A tricyclic antidepressant. At 25-50mg nightly, it helps 47% of people sleep better and feel less pain.
- Graded exercise: Start slow. Walk 5 minutes, add 10% each week. It doesn’t hurt more-it helps retrain your nervous system. Studies show 25-40% improvement in function.
- Pain neuroscience education: Learning how your nervous system works cuts fear. Patients who understand central sensitization reduce pain catastrophizing scores by 20-30%.
- Mindfulness and meditation: After 8 weeks, people report 25% less pain interference. It doesn’t erase pain-but it changes your relationship to it.
- Sleep hygiene: Fixing sleep is often the first step. No caffeine after 2pm. No screens an hour before bed. Consistent wake-up time-even on weekends.
What Doesn’t Work
Surgery? Usually not. If the pain isn’t coming from a torn ligament or pinched nerve, cutting or fixing tissue won’t help. Injections? Temporary at best. Opioids? They make central sensitization worse over time. They reduce natural pain control and increase sensitivity. And don’t fall for the "just push through" advice. Overdoing it triggers flare-ups. The goal isn’t to eliminate pain overnight-it’s to lower the volume slowly.The Diagnostic Delay Problem
Too many people wait years. A 2023 survey found 63% saw 4-6 doctors over 2-5 years before getting the right diagnosis. Why? Because most doctors aren’t trained to recognize it. Orthopedists see structural damage. Rheumatologists look for inflammation. Neurologists check for nerve damage. But central sensitization? It’s invisible on X-rays, MRIs, and blood tests. That’s why it’s mislabeled as "psychosomatic" or "fibro fog." But it’s not in your head-it’s in your nervous system.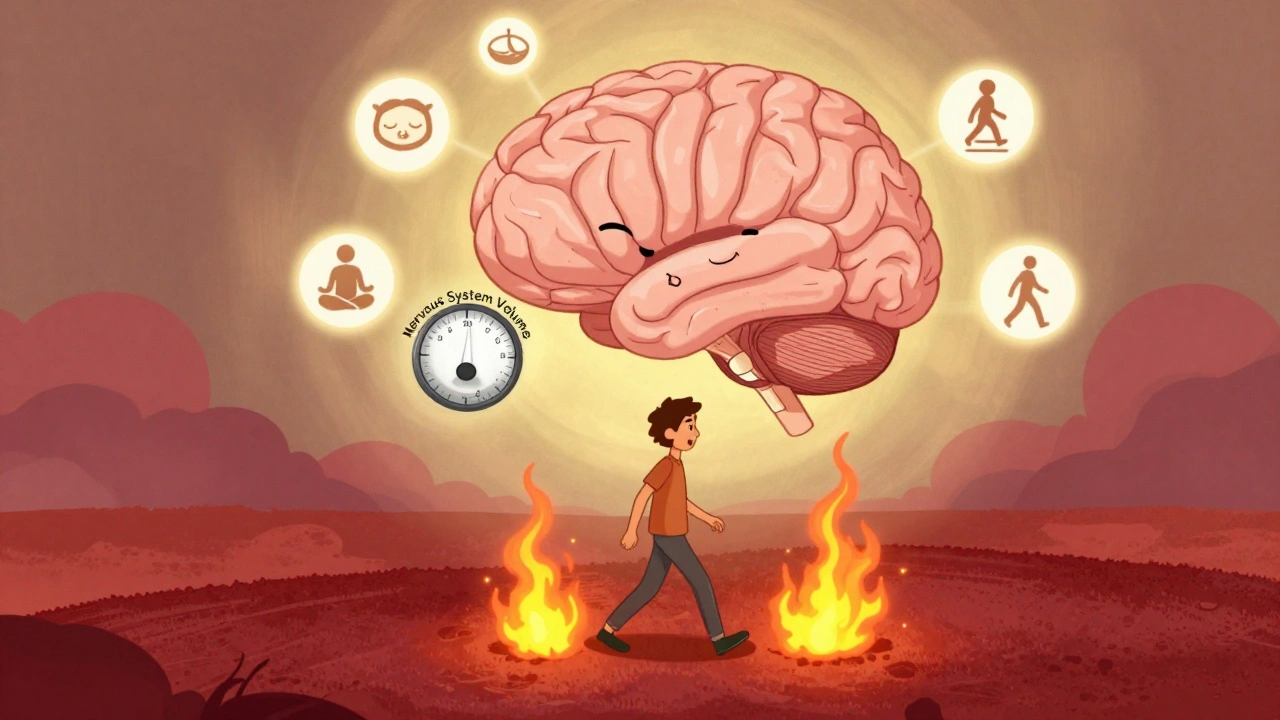
Where Is the Research Headed?
The NIH spent $63 million on central sensitization research in 2023-up from $42 million in 2018. That’s a 50% increase. Why? Because treatments are improving. New tools like standardized QST protocols from Germany now identify central sensitization with 85% accuracy. PET scans are showing reduced mu-opioid receptor binding. CSF tests reveal elevated substance P levels. Five new drugs are in Phase II trials, targeting specific molecules involved in neural hyperexcitability. Experts predict these could boost effectiveness by 30-40% in the next 5-7 years. And pain neuroscience education is now being rolled out in physical therapy programs. By 2026, half of PT clinics in the U.S. and Europe are expected to teach patients how their pain works-not just how to stretch.What This Means for You
If you’ve been told your pain is "all in your head," you’re not crazy. You’re not lazy. You’re not failing. Your nervous system got stuck. And it can be rewired. Start with education. Read about it. Talk to a pain specialist or physiotherapist trained in central sensitization. Track your triggers: what makes it worse? What helps-even a little? Movement matters. Sleep matters. Stress management matters. Medications can help-but they’re not magic. They work best when paired with retraining your brain and body. This isn’t about curing pain overnight. It’s about lowering the volume. One step at a time.Common Questions About Central Sensitization
Is central sensitization the same as fibromyalgia?
No. Fibromyalgia is a diagnosis based on widespread pain and other symptoms. Central sensitization is the underlying mechanism-what’s happening in the nervous system. About 90% of fibromyalgia patients have central sensitization, but not everyone with central sensitization has fibromyalgia. It also shows up in chronic back pain, migraines, and post-viral syndromes.
Can central sensitization go away?
Yes. It’s not permanent damage-it’s a learned response in the nervous system. When the right combination of treatments is applied-medication, movement, sleep, and education-the brain can relearn how to process signals normally. Recovery takes time, often months to years, but many people see significant improvement. Some even return to full activity.
Why do I hurt more on some days than others?
Your nervous system is sensitive to stress, sleep, weather, emotions, and even what you eat. A bad night’s sleep, a stressful meeting, or a cold day can all trigger a flare-up. It’s not because you’re doing something wrong-it’s because your system is on high alert. Tracking triggers helps you predict and manage these ups and downs.
Is it safe to exercise if everything hurts?
Yes-but it has to be gentle and gradual. Start with 5 minutes of walking or stretching. If you feel worse the next day, you went too far. The goal isn’t to push through pain, but to slowly teach your nervous system that movement is safe. Over weeks, you’ll notice your tolerance increases. Many people report less pain after consistent, low-intensity movement.
Why do doctors often miss this diagnosis?
Most doctors are trained to look for structural damage-herniated discs, arthritis, torn tendons. Central sensitization doesn’t show up on scans. It requires a different kind of evaluation: asking about pain spread, sensitivity to touch, sleep, and stress. Only about 65% of clinicians agree on the diagnosis. That’s why seeing a pain specialist or physiotherapist trained in neuroscience is key.
Next Steps
If you suspect you have central sensitization:- Find a healthcare provider familiar with pain neuroscience-rheumatologists, neurologists, or physiotherapists who specialize in chronic pain.
- Ask about quantitative sensory testing (QST) or pain drawing analysis.
- Start a simple journal: note pain levels, sleep, stress, and activities. Look for patterns.
- Try one non-drug approach: 10 minutes of walking daily, or a mindfulness app like Insight Timer.
- Avoid opioids and aggressive treatments like injections or surgery unless clearly indicated.

Comments (12)
Doug Hawk
Man i never realized how much my nervous system was just screaming all the time. That whole wind-up analogy? Perfect. I thought i was just weak but turns out my spinal cord is stuck on 11. No wonder ibuprofen does jack.
Also that bit about endorphins not working? Makes sense why i feel nothing when i take tramadol. Like my body just stopped listening.
Carolyn Woodard
The neurobiological weight of this is staggering. It’s not pathology-it’s neuroplastic maladaptation. The mu-opioid receptor downregulation, the cytokine storm in the dorsal horn, the failure of descending inhibition… it’s a perfect storm of central dysregulation. We’ve been pathologizing physiology.
And yet, the clinical community still treats this like a psychological failure. The epistemological violence here is unconscionable.
Saket Modi
so u mean my whole life of hurting for no reason is bc my brain is glitchy? lmao. guess i dont need to go to the gym after all 😂
Chris Wallace
I’ve been dealing with this for over a decade now. I used to think it was just bad luck or aging. But reading this, it’s like someone finally turned on the light in a room I’ve been stumbling around in for years. The fact that my pain spreads like a fog, that my shirt feels like barbed wire, that even a hug feels like a violation-it’s all documented here. And it’s not in my head. It’s in my neurons. That’s the first time I’ve ever felt believed.
It’s not about pushing through. It’s about rewiring. And that’s terrifying. But also… kind of hopeful.
william tao
While the scientific underpinnings are undeniably compelling, one must interrogate the underlying epistemological framework of this discourse. The conflation of neurophysiological phenomena with clinical diagnoses risks reinforcing a biomedical hegemony that pathologizes subjective experience. Furthermore, the recommendation of pregabalin-a drug with a well-documented risk profile-raises serious ethical concerns regarding pharmaceutical influence on medical practice.
One must ask: Is this truly a medical condition, or merely a socially constructed narrative?
Sandi Allen
THIS IS A LIE. THE GOVERNMENT AND BIG PHARMA ARE USING THIS TO DRUG YOU. THEY DON'T WANT YOU TO KNOW THAT PAIN IS JUST A TEST FROM GOD TO SEE IF YOU'RE STRONG ENOUGH!!
THEY'RE LYING ABOUT THE MUE-OPIOID RECEPTORS!! THEY'RE LYING ABOUT THE 20-35% INCREASE!! THEY'RE LYING ABOUT EVERYTHING!!
IF YOU'RE HURTING, PRAY MORE, EAT LESS SUGAR, AND STOP BEING A COWARD!!
THEY WANT YOU TO BELIEVE YOU'RE BROKEN SO YOU'LL TAKE THEIR DRUGS AND NEVER QUESTION THE SYSTEM!!
John Webber
i had back pain for 3 years after lifting a box. docs said its just stress. i read this and was like… wait this sounds like me. the burning, the spread, the no sleep, the fear of touch. i thought i was crazy. turns out my nerves are just broken. not my fault. thank god.
also i spelled sensitization wrong. sorry.
Shubham Pandey
So basically your brain is overreacting. Just chill.
Elizabeth Farrell
Thank you for writing this with such clarity and compassion. I’ve spent years feeling like a burden because I couldn’t ‘just push through.’ I’ve been told I’m too sensitive, too dramatic, too weak. But this? This explains the science behind my reality.
And if you’re reading this and you’ve been told your pain isn’t real-please know: you’re not broken. Your nervous system is just stuck in a loop. And loops can be undone.
Start small. One minute of walking. One deep breath. One day without guilt. Progress isn’t linear, but it’s possible. You’re not alone. I’m rooting for you.
Sheryl Lynn
How quaint. A beautifully articulated exposition on the neurophenomenology of somatosensory hyperexcitability-truly a masterpiece of clinical poetry. One almost forgets we’re living in the age of algorithmic diagnostics and AI-driven pain mapping.
Yet, one wonders: does the mere articulation of this phenomenon, however elegantly rendered, not merely reinforce the very biopolitical apparatus that commodifies suffering? I mean, is this not just another neoliberal narrative of self-optimization wrapped in neuroscientific velvet?
Paul Santos
Love this. The wind-up analogy? Chef’s kiss. 🤙
Also, low-dose naltrexone? That’s the secret sauce. I’ve been on it for 18 months. My pain dropped from a 9 to a 3. Not cured. But now I can sleep. And that’s everything.
Also, if you’re reading this and you’re still on opioids? Stop. They’re making it worse. I learned the hard way.
Eddy Kimani
Just wanted to add-this isn’t just about pain. It’s about being seen. I’ve been told I’m exaggerating, that I’m anxious, that I need to ‘get over it.’ But when you realize your nervous system is literally rewired by trauma, stress, and inflammation… it’s not weakness. It’s biology.
And if you’re out there feeling invisible? You’re not. We’re here. We’re real. And we’re learning how to turn the volume down. One step, one breath, one gentle movement at a time.