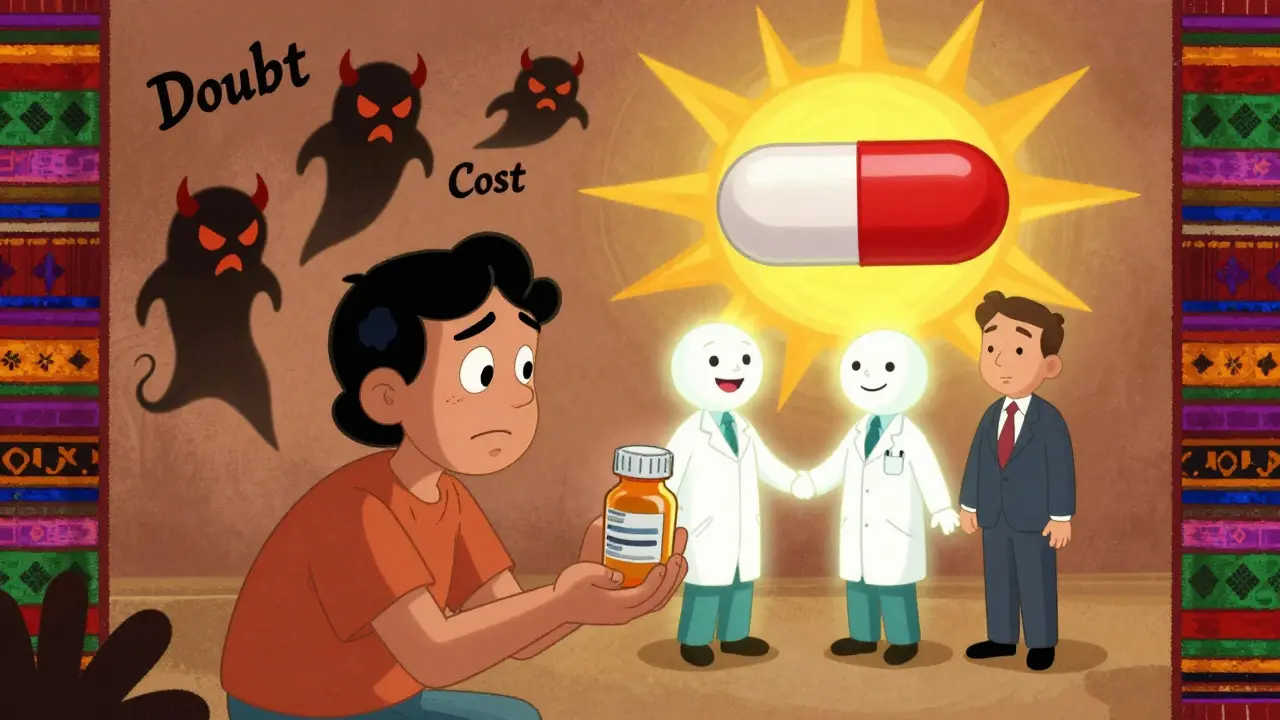
For most people, switching from a brand-name drug to a generic feels like a gamble. You’ve been taking the same blue pill for years. The box has your doctor’s name on it. The pharmacy knows you by name. Then one day, the bottle looks different. The pill is white. The label says something else. You’re told it’s the same thing. But is it?
The truth is, 9 out of 10 prescriptions filled in the U.S. today are generics. They’re not cheaper because they’re worse. They’re cheaper because the patent expired. The FDA requires them to have the same active ingredient, dose, strength, and route of use as the brand-name version. They must also prove they work the same way in the body-within a tight 80% to 125% range of absorption. That’s not guesswork. That’s science. And yet, nearly a third of patients still believe generics are less effective or more likely to cause side effects.
Why does this gap exist? Because confidence isn’t built by brochures or websites. It’s built in conversations-short, honest, and repeated. Research shows that when a doctor or pharmacist takes just two to three minutes to explain what generics are and why they’re safe, patient acceptance jumps from 63% to over 84%. That’s not a small win. That’s life-changing for people who skip doses because they’re afraid.
What Patients Really Think About Generics
A 2024 study published in PLOS ONE surveyed over 2,000 Americans and found that 49.4% believe doctors should prescribe more generics. But only 37.6% of patients actively prefer them. That disconnect tells you something important: people don’t oppose generics because they’re irrational. They oppose them because they’ve never been given clear, trustworthy information.
Let’s break down the real concerns:
- 24.1% worry the generic won’t control their condition as well.
- 25.7% just don’t want to change-"If it ain’t broke, don’t fix it."
- 29.5% fear new side effects, even if they’ve never had them before.
- 20.8% say they’d rather pay more for peace of mind.
These aren’t irrational fears. They’re rooted in real experiences. One Reddit user, u/MedUser88, wrote about switching from brand-name Sertraline to a generic and suddenly feeling jittery and nauseous. The brand version had worked perfectly for three years. The generic didn’t. Was it the drug? Or was it the filler? The FDA allows different inactive ingredients in generics-things like dyes, binders, or coatings. These don’t affect how the medicine works, but they can trigger reactions in people with sensitivities. That’s not a failure of the generic. It’s a reminder that every body reacts differently.
Another big issue: appearance. A pill that looks different feels different. A patient who’s been on a specific brand for years might associate the color, shape, or size with "feeling better." When that changes, even if the science says it’s identical, their body doesn’t know that. They feel like something’s off. And when they feel off, they blame the medicine-not their own expectations.
Who’s Most Likely to Doubt Generics-and Why
Not everyone doubts generics equally. Research shows clear patterns:
- Patients with low health literacy are twice as likely to believe generics are less safe.
- People on Medicaid report higher skepticism than those with private insurance.
- Non-white patients show lower confidence levels-just 78.3% trust generics, compared to 89.1% of white patients.
- Those with lower income or less education are more likely to assume cost equals lower quality.
These aren’t random. They’re the result of systemic gaps. If you’ve never had a doctor sit down with you to explain how drugs are approved, if you’ve been handed a pill bottle with no context, if your pharmacy visits are rushed and transactional-you’re more likely to assume the worst.
And here’s the kicker: older adults are actually the most confident. A 2014 NIH study found that 71.4% of patients over 60 believed generics were safe. Why? Because they’ve seen more. They’ve watched their prescriptions change over decades. They’ve learned that the system works. They’ve trusted their pharmacists. That’s not luck. That’s experience.
The Power of the Pharmacist’s Voice
Pharmacists are the most underused tool in building patient confidence. They’re the last person a patient talks to before swallowing the pill. And they’re the only one legally allowed to explain substitution.
Here’s what works:
- Instead of saying, "This is the generic version," say: "This is the same medicine you’ve been taking, just made by a different company after the patent expired. The FDA checks it just as closely as the brand name. It’s been used by over 100,000 people in this country without any safety issues."
- Use the Newest Vital Sign test-a quick, three-question tool that helps you gauge if a patient understands basic health terms. If they struggle, simplify. No jargon. No "bioequivalence." Say: "It works the same way in your body. The FDA won’t let it be sold unless it does."
- Ask open questions: "What’s your biggest concern about switching?" Then listen. Don’t interrupt. Don’t correct. Just hear them.
- Hand them a printed fact sheet from the FDA’s website. Not a glossy pamphlet from the drugmaker. The FDA’s own page, updated in October 2023, answers 50 common questions in plain language.
One study found that patients who received even a short explanation from their pharmacist were 36% more likely to say they were comfortable with the switch. That’s not because they suddenly became scientists. It’s because they felt respected.

What Doctors Can Do (Without Extra Time)
Doctors don’t need to spend 10 minutes on this. They just need to say the right thing once.
Here’s a script that works:
"I’m switching you to the generic version of this medicine because it’s just as effective, and it’ll save you a lot of money. The FDA makes sure it’s identical in how it works. Some people notice a small difference in how the pill looks, but that doesn’t mean it’s different inside. If you feel anything unusual after switching, let me know. But most people don’t notice a thing."
That’s it. Two minutes. No fluff. No fear.
And here’s something powerful: when a doctor says, "I prescribe generics to my own family," trust spikes. Patients don’t just want facts. They want reassurance that the person giving them advice believes in it too.
Why the FDA’s Role Matters More Than You Think
The FDA doesn’t just approve generics. It polices them. Every batch of every generic drug is tested for purity, strength, and stability. The same factories that make brand-name drugs often make the generics. The only difference? No marketing budget.
But most patients don’t know that. They think generics are made in some back-alley lab. They don’t realize the FDA inspects every facility-whether it’s in the U.S., India, or Germany. They don’t know that 92.7% of all Medicare Part D prescriptions are generics-and that number keeps rising because the system works.
So when you talk to a patient, say this: "The FDA holds generics to the same exact standards as brand-name drugs. If a generic doesn’t work the same way, it doesn’t get sold. That’s not a suggestion. That’s the law."
What Doesn’t Work
Don’t rely on pamphlets alone. A 2023 study found that 62% of patients found pharmacy handouts "somewhat helpful" at best. They’re ignored.
Don’t assume patients know what "bioequivalence" means. Most don’t. And if you use the word, you’ve lost them.
Don’t say, "It’s the same thing." That’s too vague. Say: "Same active ingredient. Same dose. Same effect. Different company. Same FDA approval."
Don’t make it sound like a cost-cutting trick. Frame it as a smart, science-backed choice.
Real Stories, Real Results
In a clinic in rural Ohio, nurses started using a simple script before handing out new prescriptions: "This is the generic version of your medicine. It’s the same, just cheaper. We’ve had over 200 patients switch, and 98% say they feel the same. If you don’t, come back. We’ll switch you right away."
Within six months, refill rates for generics went up by 19%. No one got sicker. No one complained. People just felt heard.
At a CVS in Phoenix, a pharmacist started asking every patient who picked up a generic: "Have you ever taken this medicine before? What did you think?" That simple question opened conversations. One man, 72, said he’d refused generics for years because he thought they were "cheap knockoffs." The pharmacist showed him the FDA website on his phone. He nodded. "I just didn’t know," he said. He’s been on the generic since.
The Bottom Line
Generics aren’t a compromise. They’re a victory. They’ve saved Americans $370 billion in one year. They’ve kept millions of people on their medications because they could afford them. And they’re just as safe, just as effective, and just as regulated as the brand names.
The only thing standing between patients and confidence? A few minutes of clear, kind, honest conversation.
It’s not about changing minds. It’s about removing fear. And that starts with one person-your doctor, your pharmacist, you-saying the right thing at the right time.


Comments (14)
Virginia Seitz
I just switched to generic sertraline and felt like a robot for a week 😅 but then I realized it was my brain adjusting. Same pill, different wrapper. We overthink meds.
Salome Perez
The FDA’s standards for generics are among the most rigorous in the world. Every batch undergoes dissolution testing, potency verification, and stability monitoring. The notion that generics are "second-rate" is a myth perpetuated by marketing, not science. Patients deserve transparency-not fear.
Victoria Rogers
Generics are a socialist plot to make Americans take cheap drugs from China. My grandpa died because he took a knockoff heart med. I know people who know people.
Patrick A. Ck. Trip
It's fascinating how deeply psychological the perception of medication is. The color, shape, and even the smell of a pill can trigger placebo or nocebo responses. Science tells us they're equivalent-but the mind doesn't always listen. That’s why communication matters more than data.
Nishant Desae
I come from India, where generics are the backbone of healthcare. We don’t have the luxury of brand-name drugs. But here’s the thing-our pharmacists are trained to explain everything. They don’t just hand over the bottle. They sit down. They ask, "How did you feel on the last one?" They show you the FDA page on their phone. And guess what? People trust them. It’s not about money. It’s about dignity. In the U.S., you treat patients like customers. In places like mine, you treat them like family.
Kaylee Esdale
my pharmacist just said "same stuff different box" and i believed her. no jargon no stress just truth
Jody Patrick
Generic manufacturers are owned by Big Pharma anyway. You’re being played.
Erik J
I’ve been on a generic for hypertension for 4 years. My BP is stable. My co-pay is $3. I’ve never had a side effect. But I still feel guilty taking it. Like I’m cheating the system. Why does that happen?
BETH VON KAUFFMANN
The bioequivalence range of 80–125% is not a scientific standard-it’s a regulatory compromise. A 25% variance in absorption is clinically significant for narrow-therapeutic-index drugs like warfarin or levothyroxine. The FDA’s data is cherry-picked. Real-world studies show higher failure rates in elderly polypharmacy patients.
Chris Van Horn
The assertion that generics are "just as effective" is not only scientifically reductive, but epistemologically negligent. The FDA’s bioequivalence protocol, predicated upon Cmax and AUC metrics, fails to account for inter-individual pharmacokinetic variability, particularly in polymorphic CYP450 metabolizers. Moreover, the inclusion of non-active excipients-such as lactose monohydrate, magnesium stearate, and FD&C dyes-introduces confounding variables that are neither standardized nor transparently disclosed. One cannot equate chemical identity with therapeutic equivalence. This is not skepticism; it is epistemic rigor.
Sam Clark
I’ve worked in community pharmacy for 18 years. I’ve seen patients cry because they think the generic won’t work. I’ve seen them get better because we took two minutes to explain. It’s not about the pill. It’s about the pause. The eye contact. The "I’ve been where you are." That’s the real medicine.
Martin Spedding
Generics are a scam. I work in a lab. I’ve seen the batches. The fillers are junk. The FDA is asleep at the wheel. This whole system is rigged.
Evelyn Vélez Mejía
There is a profound ethical tension here: we demand cost-efficiency in healthcare while simultaneously denying patients the psychological security that comes with familiarity. The brand-name drug is not merely a chemical compound-it is a symbol of continuity, of control, of trust. To dismiss the emotional architecture of medication adherence as mere superstition is to misunderstand the human condition. We do not treat diseases. We treat people who are afraid.
Meghan O'Shaughnessy
I switched to generic omeprazole after my insurance forced it. Felt fine. Then I saw the pill was a different shade of purple. I Googled it. Found a Reddit thread from 2017 where someone said they got migraines from the new version. I stopped taking it. My reflux came back. I didn’t switch back. I just suffered. That’s the problem. We don’t get follow-up. We get a bottle and a silence.