Why Your Medications Expire Sooner Than They Should
You bought that painkiller, antibiotic, or heart medication with a date on the bottle - but it didn’t last that long. Maybe it lost its punch. Maybe it started smelling weird. Or maybe you just threw it out because you weren’t sure if it was still safe. The truth? Most medications don’t expire because they go bad on their own. They expire because they’re stored wrong.
The U.S. Food and Drug Administration says expiration dates aren’t arbitrary. They’re based on real testing. A drug is guaranteed to stay at 90-110% of its labeled strength until that date - if it’s kept under the right conditions. But here’s the problem: 37% of premature medication expirations in homes are caused by bad storage, according to the CDC. And humidity? That’s the biggest killer. Bathrooms are the worst place for meds. Showers spike humidity to 95%. That’s like putting your pills in a steam room every morning.
Where NOT to Keep Your Medications
Stop putting meds in the bathroom cabinet. Seriously. It’s the most common mistake. The heat and moisture from showers break down aspirin 300% faster than in dry air. Even your kitchen isn’t safe. Near the stove? Temperature swings can jump 15°C in under 30 minutes. That’s enough to ruin antibiotics, thyroid meds, and insulin before their expiration date.
Don’t leave pills in the car. Summer temps inside a parked car can hit 60°C. Winter? Freezing can crack liquid vials or make tablets crumble. And don’t stash them in a dresser drawer unless you’re sure it’s cool and dry. A drawer in a humid basement? Just as bad as the bathroom.
And no, the fridge isn’t always the answer. Only put meds in the fridge if the label says so. Putting a pill that’s meant for room temperature into the fridge can cause condensation. Water droplets form inside the bottle. That’s moisture - and moisture = degradation.
Where You SHOULD Store Your Medications
The best spot? A cool, dry place - away from windows, heat vents, and sinks. A bedroom drawer, a closet shelf, or a dedicated cabinet in a central part of your home works best. Ideal temperature? Between 20-25°C (68-77°F). Humidity? Below 60%. You don’t need fancy gear, but a simple digital hygrometer (costs under $10) can tell you if your storage spot is safe.
Keep everything in the original container. That amber bottle? It blocks 97% of UV light. Clear plastic? Not so much. Light degrades medications like nitroglycerin, birth control pills, and seizure drugs. The original label also has the expiration date, dosage, and warnings. If you transfer pills to a pill organizer, keep the original bottle nearby. Don’t toss it.
Special Cases: What to Do With Insulin, Eye Drops, and Other Sensitive Drugs
Not all meds are created equal. Some need special treatment.
- Insulin: Unopened? Refrigerate at 2-8°C. Once opened? It can stay at room temperature (up to 25°C) for up to 28 days. Check the package insert - some newer types last longer.
- Nitroglycerin: Must stay in its original dark glass bottle. Even a clear pill case will ruin it. And don’t open it unless you need it - exposure to air reduces potency.
- Eye drops: Once opened, most last only 28 days. After that, they can grow dangerous bacteria like Pseudomonas. Even if the expiration date is months away, toss it after four weeks.
- Refrigerated liquid antibiotics: Keep them in the center of the fridge, not the door. Door shelves swing in temperature every time you open it. That’s bad for stability.
How to Tell If a Medication Has Gone Bad
Expiration dates are a guide, but your eyes and nose can tell you more.
- Smell: Aspirin that smells like vinegar? That’s acetylsalicylic acid breaking down. Don’t take it.
- Color: Tablets or capsules that are darker, lighter, or have spots? Throw them out. A 15% color change is a red flag.
- Texture: Pills that crumble, stick together, or feel oily? Not safe. Liquids that are cloudy, thick, or have floating particles? Discard.
- Odor: Any unusual smell - chemical, sour, moldy - means something’s wrong.
When in doubt, don’t guess. Call your pharmacist. They’ll tell you if it’s still safe - and often for free.
Organization Tips That Actually Work
Keeping track of expiration dates is easier than you think.
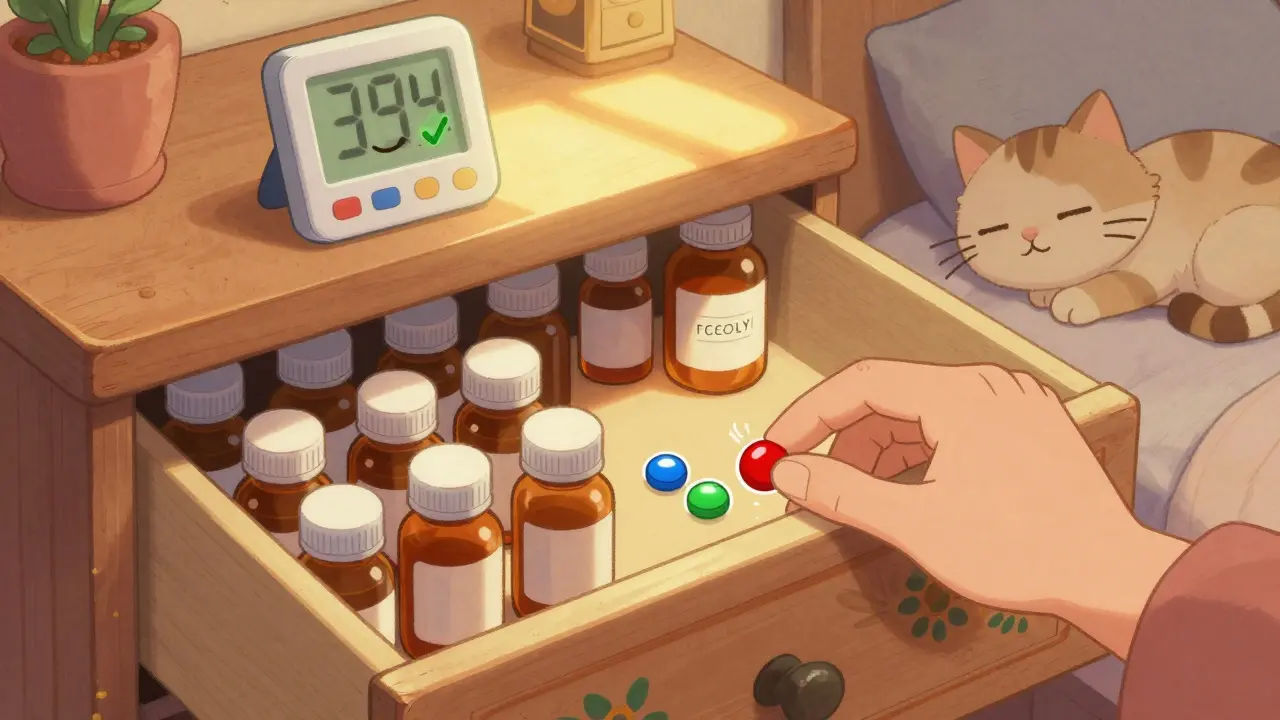
Use a color-coded system: red dots for meds expiring this year, blue for next year, green for two years out. One study at the University of Wisconsin found this cut expired meds by 63%. You can buy sticker packs online or just use colored tape.
Assign one person in the household to check meds monthly. Just 10 minutes a month catches 89% of problems before they become risks. Make it part of your routine - like checking the smoke detector.
Store all meds in one locked cabinet. Not just prescription drugs - OTC painkillers, vitamins, supplements. This keeps them away from kids and pets, and makes it easier to monitor. A cabinet with a built-in thermometer and hygrometer? Even better. Some smart pillboxes now track temperature and humidity and send alerts to your phone.
What About Expired Meds? Can You Still Use Them?
The FDA’s Shelf Life Extension Program found that 90% of military stockpiled drugs stayed potent 15+ years past expiration - but only because they were stored in climate-controlled vaults. That’s not your medicine cabinet.
For most people, expired meds are risky. Antibiotics may lose potency and fail to treat infections. Insulin might not lower blood sugar. Epinephrine auto-injectors (EpiPens) can become ineffective in emergencies. That’s not worth the gamble.
There’s one exception: if you’re in a remote area, with no access to a pharmacy, and you’re out of a life-saving drug like insulin or an EpiPen - and it’s only a few months past expiration - some experts say using it is better than nothing. But that’s a last-resort emergency call, not a routine practice.

How to Dispose of Old or Expired Medications Safely
Don’t flush them. Don’t toss them in the trash. Don’t pour them down the sink.
The safest way? Use a drug take-back program. The DEA runs National Prescription Drug Take Back Day twice a year. In 2024, over 11,000 collection sites will be open - pharmacies, police stations, hospitals. You can drop off anything: pills, patches, liquids. No questions asked.
If there’s no take-back event near you, mix pills with coffee grounds or cat litter in a sealed bag, then throw them in the trash. This makes them unappealing and unusable. Remove labels from bottles to protect your privacy.
What’s Changing in Medication Storage?
Pharmaceutical companies are starting to design better drugs. Merck’s new heat-stable insulin can stay at 30°C for 56 days - a big win for people in hot climates or without reliable refrigeration.
Prescription labels now often include icons: a snowflake for refrigeration, a sun with a line through it for light sensitivity. More than 78% of new labels have these now.
And new tech is coming. University of Wisconsin is testing prescription bottles with built-in silica gel to keep humidity low. The FDA is also looking at real-time expiration indicators - tiny sensors that change color when a drug degrades.
But until then? The best tool you have is knowledge. Store meds right. Check them often. Dispose of them safely. It’s not complicated. It just takes a little attention.
Final Thought: Your Health Depends on It
Medications aren’t like milk. You can’t just smell them and know they’re bad. But they’re just as fragile. A pill that’s lost its strength won’t help your blood pressure. A degraded antibiotic won’t kill the infection. And a weak EpiPen could cost you your life.
Proper storage isn’t about being perfect. It’s about being smart. Keep meds cool, dry, and in their original bottles. Check them every month. Toss anything that looks or smells wrong. Use take-back programs. You’re not just saving money - you’re protecting your health, and the health of everyone in your home.
Can I store medications in the bathroom?
No. Bathrooms are too humid and hot. Showers can raise humidity to 95%, which breaks down pills and liquids faster. The CDC says humidity is the top cause of premature medication expiration in homes. Store meds in a cool, dry place like a bedroom drawer or closet instead.
Do all medications need to be refrigerated?
No. Only medications that specifically say "refrigerate" on the label need to be kept cold - like insulin, some antibiotics, and eye drops. Putting other pills in the fridge can cause condensation, which introduces moisture and damages them. Always check the label or ask your pharmacist.
How do I know if my medicine has gone bad?
Look for changes: tablets that are discolored, cracked, or sticky; liquids that are cloudy or have particles; pills that smell like vinegar (aspirin) or chemicals. If anything looks, smells, or feels off, don’t take it. When in doubt, call your pharmacist.
Can I use expired medication in an emergency?
Generally, no. Expired insulin, EpiPens, or antibiotics may not work when you need them most. While some drugs stored perfectly in labs stay potent for years, household conditions are never perfect. Using expired meds is risky - only consider it if you’re stranded with no access to a pharmacy and it’s a life-or-death situation.
Where can I safely dispose of old meds?
Use a DEA National Prescription Drug Take Back Day collection site - there are over 11,000 locations nationwide, including pharmacies and police stations. If no event is nearby, mix pills with coffee grounds or cat litter in a sealed bag and throw them in the trash. Never flush them.
Do smart pillboxes really help with storage?
Yes. Devices like MedMinder Pro monitor temperature and humidity inside the container and alert you if conditions get unsafe. They’re especially helpful for high-risk meds like insulin or nitroglycerin. While not necessary for everyone, they add a layer of protection if you live in a hot or humid climate.


Comments (13)
LIZETH DE PACHECO
I used to keep my meds in the bathroom until my grandma called me out on it. She said, 'Honey, if you want your pills to work, stop treating them like your toothpaste.' Now I have a little drawer in my bedroom with a silica gel pack. Best decision ever.
Lee M
Let’s be real - the FDA doesn’t care if your aspirin turns to vinegar. They just want you to buy new ones. The real expiration date is when your wallet says so. I’ve taken pills 3 years past their date and lived to tell the tale. Stop fearmongering.
Kristen Russell
My mom does the color-coded sticker thing and it’s genius. Red = this year, blue = next. She checks every Sunday with her coffee. Simple. Effective. No drama.
Bryan Anderson
The scientific consensus is clear: environmental factors significantly impact pharmaceutical stability. Humidity, thermal cycling, and photodegradation are well-documented mechanisms of degradation. Storing medications in a climate-controlled environment is not merely recommended - it is pharmacologically prudent.
Matthew Hekmatniaz
I’m from Iran and we don’t have AC in most homes. We keep meds in sealed jars with rice inside - absorbs moisture. Works better than you think. Also, never store near the stove. My uncle’s blood pressure meds turned to powder. He didn’t know until he collapsed.
Liam George
You think this is about storage? Nah. The pharma companies *want* you to throw out meds early. That’s why expiration dates are set so aggressively. They’re not testing for safety - they’re testing for profit. The government knows. They just won’t say it. The Shelf Life Extension Program proves it. 15+ years? Yeah. But you’ll never see that on your bottle.
Dusty Weeks
i just throw mine in the fridge lol who cares if it gets a lil moist its fine 🤷♂️💊
Sally Denham-Vaughan
I keep my meds in a shoebox under my bed. Cold, dark, dry. No one touches it. My cat doesn’t even know it’s there. Simple. Works. No tech needed.
Richard Thomas
There’s an interesting philosophical tension here between human impermanence and the illusion of pharmaceutical permanence. We treat pills like they’re eternal objects, but they’re not - they’re chemical systems in dynamic equilibrium with their environment. The expiration date is a social contract, not a biological law. And yet, we cling to it as if it were scripture. We fear the unknown potency more than we fear the known risk of non-adherence. Isn’t that ironic? We’re terrified of a pill losing strength, but we’re perfectly comfortable letting our own health decay through inaction. The real expiration date isn’t on the bottle - it’s on the calendar of our discipline.
Paul Ong
Just put your meds in a drawer and forget about it. If it looks weird toss it. If it looks fine keep going. Life’s too short to stress over pill boxes
Andy Heinlein
I got one of those smart pillboxes last year and honestly it changed my life. My mom has diabetes and she forgets stuff. Now she gets a text if it’s too hot or too cold. Also it reminds her to take her meds. She says she feels like she’s got a little nurse in her pocket. Best $80 I ever spent.
Ann Romine
I’m curious - do any of the new heat-stable insulins work for people who live in places without refrigeration? My cousin in rural Texas has to drive 40 miles for refills. If these new ones can sit in a car for days, that’s huge.
Todd Nickel
The CDC’s statistic about 37% of premature expirations being due to improper storage is statistically significant, but it’s also a product of confirmation bias in data collection. Most participants in such studies are middle-class Americans with access to climate-controlled homes - so the data reflects a narrow demographic. In many parts of the world, including low-income urban areas in the U.S., the primary constraint isn’t bathroom humidity - it’s the lack of any dedicated storage space at all. People store meds in plastic bags in coat pockets, under sinks, or even in purses. The real issue isn’t education - it’s infrastructure. Until we address housing conditions, temperature control, and access to sealed containers, all the advice in the world won’t fix the root problem.