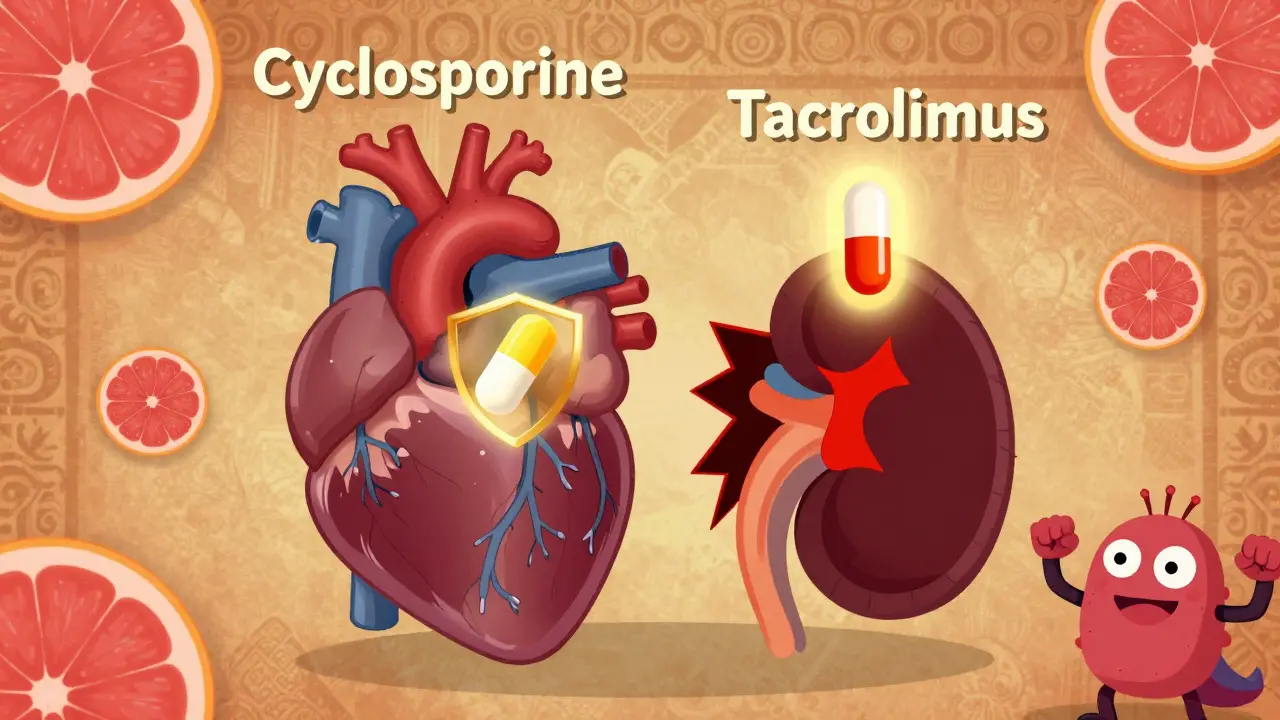
When someone gets a kidney, liver, or heart transplant, their body’s natural defense system tries to reject the new organ. To stop that, they need powerful drugs-cyclosporine and tacrolimus. These aren’t just any pills. They’re narrow therapeutic index drugs, meaning the difference between a dose that works and one that causes harm is razor-thin. And now, with generics dominating the market, things have gotten a lot more complicated.
Why These Drugs Are So Tricky
Cyclosporine and tacrolimus both work the same way: they block a protein called calcineurin, which tells immune cells to attack. But that’s where the similarity ends. Tacrolimus is about 20 to 100 times more potent than cyclosporine. A typical daily dose of tacrolimus is around 5 mg, split into two doses. Cyclosporine? You’re looking at 150 mg or more, twice a day. Even small changes in how your body absorbs these drugs can mean the difference between rejection and toxicity.
Therapeutic levels are strict. For tacrolimus, blood levels need to stay between 5 and 15 ng/mL in the first few months after transplant. Go below 5? Your body might start attacking the new organ. Go above 15? You risk kidney damage, tremors, or even seizures. Cyclosporine’s range is wider-100 to 200 ng/mL-but still tight enough that a 10% shift can cause problems.
Both drugs are broken down by the same liver enzyme, CYP3A4. That means grapefruit juice, certain antibiotics, or even changes in your diet can throw off your levels. And if you switch from one generic version to another? That’s when things get risky.
The Rise of Generics-and the Hidden Risks
By 2023, over 92% of tacrolimus and cyclosporine prescriptions in the U.S. were generics. That’s good news for wallets. Brand-name Prograf (tacrolimus) used to cost $1,200 to $1,500 a month. Generic versions? $300 to $500. Neoral (cyclosporine) dropped from $800 to $1,000 down to $150 to $300. For many patients, that’s the difference between staying on medication and skipping doses.
But here’s the catch: not all generics are created equal. The FDA says a generic must deliver 80% to 125% of the active ingredient compared to the brand. Sounds tight? It’s not. For a drug with a narrow therapeutic index, that 45% window is huge. One generic might deliver 90% of the expected dose. Another might deliver 115%. That’s not just a difference in cost-it’s a difference in survival.
Real patients have felt it. One transplant recipient on Reddit reported his tacrolimus levels dropped from 8.5 to 5.2 ng/mL within two weeks after switching to a new generic. He ended up in the hospital with mild rejection. Another user said his nephrologist refuses to let him switch generics because his levels “never stabilized” after the first try.
Who’s Affected Most?
It’s not just about cost. It’s about consistency. Studies show that patients who switch between different generic brands are 15% more likely to miss doses or have unstable drug levels. Why? Because each manufacturer uses different fillers, binders, and coating methods. These don’t change the active ingredient-but they change how fast the drug dissolves in your gut.
For cyclosporine, the problem is worse. Older versions were oil-based and absorbed poorly. The newer microemulsion (CsA-ME) improved things, but even then, generics from different companies show up to 30% variation in absorption. That’s why some transplant centers now insist on using only one generic brand for each patient-no switching.
And it’s not just U.S. patients. The European Medicines Agency warned in 2020 that switching between generic tacrolimus products without monitoring could lead to rejection or toxicity. In 2024, they updated their guidelines to require testing in actual transplant patients-not just healthy volunteers-to prove bioequivalence.

What Happens When Levels Shift?
Imagine your body is a house. The drugs are the locks. Too little? The lock doesn’t engage-invaders (your immune system) walk right in. Too much? The lock jams-and you get side effects like kidney damage, high blood pressure, or diabetes. Tacrolimus is especially linked to new-onset diabetes after transplant, affecting nearly 20% of users. Cyclosporine? It’s more likely to cause gum overgrowth, hirsutism, and high cholesterol.
A 2022 survey of over 1,200 transplant patients found that 42.7% noticed side effects change after switching to generic immunosuppressants. Nearly one in five needed a dose adjustment. That’s not a coincidence. It’s biology.
Some patients report no issues. One person on HealthUnlocked said their levels stayed stable for 18 months after switching to generic tacrolimus-and saved $900 a month. That’s the good side. But those stories are the exception, not the rule.
How to Stay Safe
If you’re on either of these drugs, here’s what actually matters:
- Stick with one generic brand. If your pharmacy switches your prescription, ask for the same manufacturer. Don’t let them change it without telling you.
- Test your blood levels every week for the first month after any switch. Transplant centers recommend this. It’s not optional.
- Avoid grapefruit, Seville oranges, and pomegranate juice. They interfere with how your body processes these drugs.
- Take your pills at the same time every day. Even a 2-hour delay can cause fluctuations.
- Know your target range. Ask your transplant team what your ideal level is. Write it down.
Some clinics now use pharmacogenetic testing-checking your CYP3A5 gene-to predict how fast you’ll metabolize tacrolimus. A 2023 study in JAMA Internal Medicine showed this cut the time to reach stable levels by 63%. It’s not available everywhere yet, but it’s coming.
The Bigger Picture
Tacrolimus has largely replaced cyclosporine because it’s more effective. In one major study, patients on tacrolimus had half the rate of acute rejection compared to those on cyclosporine. Graft survival was better. But the cost savings come with a trade-off: more monitoring, more anxiety, more risk.
By 2024, 86% of new kidney transplant patients in the U.S. were on generic tacrolimus. That’s progress. But the International Transplant Society’s 2024 position statement put it plainly: “Generic immunosuppressants provide essential cost savings, but their narrow therapeutic index requires individualized management and avoidance of unnecessary switching.”
It’s not about avoiding generics. It’s about controlling them. If you’re on one, don’t assume it’s safe just because it’s cheap. Your life depends on consistency.
Can I switch between different generic versions of tacrolimus?
Switching between different generic versions of tacrolimus is not recommended without close monitoring. Even small changes in formulation can cause your blood levels to drop or spike, increasing the risk of rejection or toxicity. Most transplant centers require weekly blood tests for at least four weeks after any switch. Always talk to your transplant team before making any changes.
Why is tacrolimus more commonly used than cyclosporine today?
Tacrolimus is more effective at preventing acute rejection and leads to better long-term kidney function. Studies show rejection rates are nearly half with tacrolimus compared to cyclosporine. It’s also easier to dose precisely because it’s more potent. While it has higher risks of diabetes and tremors, the overall transplant outcomes are better, so it’s become the standard first-line drug.
Do generic immunosuppressants work as well as brand-name drugs?
For many people, yes. But because these drugs have a narrow therapeutic index, even small differences in absorption can matter. FDA allows generics to vary by up to 25% in how much drug enters your bloodstream. That’s acceptable for most medications-but not for transplant drugs. Some patients do fine switching. Others have rejection episodes. Consistency matters more than cost.
What should I do if I notice new side effects after switching to a generic?
Contact your transplant team immediately. New tremors, headaches, nausea, or changes in urine output could signal unstable drug levels. Your doctor will likely order a blood test to check your tacrolimus or cyclosporine concentration. Don’t wait. Even mild rejection can damage your transplant if not caught early.
Is there a way to avoid generic switching altogether?
Yes. Ask your transplant center if they have a contract with a single generic manufacturer. Many major centers now do this to prevent switching. You can also ask your insurance for a prior authorization to keep your current generic brand. Some patient advocacy groups help with appeals if your insurer forces a change.
What’s Next?
A new extended-release version of tacrolimus, approved in late 2023, may reduce fluctuations and make switching less risky. But until then, the rule is simple: know your drug, know your levels, and never switch without talking to your care team. Your transplant is too important to leave to chance.

Comments (12)
Rachidi Toupé GAGNON
Life after transplant is wild, but hey - at least we got generics that don’t bankrupt us 😊. I switched to a new brand last year and my levels stayed solid. Just stick to one, track your numbers, and don’t let pharmacies play roulette with your kidney. You got this! 🙌
Sophia Nelson
This whole thing is a scam. Pharma companies know exactly how to exploit this loophole. FDA lets generics vary by 45%? That’s not approval - that’s a death sentence waiting to happen. They’re gambling with people’s lives for profit. Someone should sue.
Reggie McIntyre
I love how this post breaks it down like a medical thriller. Tacrolimus isn’t just a drug - it’s a tightrope walk. One day you’re fine, next day your levels drop like a rock because some pharmacist swapped your bottle. I used to think generics were all the same. Nope. Now I have a spreadsheet. Yes, really. 📊
Carla McKinney
You say 'stick to one brand' like it's simple. Insurance companies force switches. Pharmacies don't ask. Transplant centers are understaffed and can't monitor everyone. This isn't a patient problem - it's a systemic failure. And no, 'just test weekly' isn't a solution when you work two jobs and have no PTO.
Ojus Save
i read this whole thing and my brain is like... huh? i just take my pill and hope for the best. i dont even know what CYP3A4 is. but i know if i miss a dose i feel like death. so yeah. dont switch. dont change. just keep the same bottle. lol
Neha Motiwala
I knew it. I KNEW IT. The government is letting this happen because they want transplant patients to die quietly. Why else would they allow such a huge window? Someone is getting rich off this. Big Pharma, the FDA, the pharmacies - all in cahoots. My cousin’s brother’s neighbor had to go back on dialysis after a switch. It’s not a coincidence.
Alyssa Williams
You’re not alone. I’m here for you. If you’re on generic tacrolimus, you’re a warrior. Every time you take that pill, you’re choosing life. Don’t let the system make you feel small. Ask for your brand. Document everything. And if your pharmacy switches it? Call them. Call your doctor. Call your senator. You have power. You’re not just a patient - you’re a force.
Jack Havard
Funny how everyone acts like this is new. Generics have been dodgy since the 90s. The FDA approval process for these drugs is a joke. They test on healthy volunteers who don’t have scar tissue, liver damage, or gut inflammation. Real patients? Afterthoughts. This isn’t about cost - it’s about convenience for bureaucrats.
Vamsi Krishna
I’ve been on cyclosporine for 11 years. I’ve switched generics six times. My levels? Like a rollercoaster with no brakes. My nephrologist says 'it’s fine' - but I’ve had two hospitalizations. I’m not complaining. I’m just saying - if you’re not monitoring like a hawk, you’re playing Russian roulette with your new organ. And someone’s laughing all the way to the bank.
Brad Ralph
So we’re saying the system is designed to kill people slowly? 🤔 I mean… if you think about it, it’s almost poetic. We save lives with science, then undermine them with bureaucracy. The irony is thick enough to spread on toast. Maybe the real transplant is the one we need in our healthcare system.
christian jon
I can't believe people are still falling for this. The FDA is a puppet of Big Pharma. They approve generics based on lab rats, not real people. And then they say 'it's bioequivalent' - but bioequivalent to what? A healthy 25-year-old? My body isn't a lab. My gut is scarred. My liver is tired. My immune system is on high alert. This isn't science - it's corporate negligence. And they call it 'affordable medicine'? No. It's affordable death.
Autumn Frankart
This is why America is crumbling. We let corporations decide who lives and who dies. If you can't afford to pay for the brand name, you're basically signing a death warrant. And don't even get me started on how the government lets foreign manufacturers make these pills. Half of them are made in places with zero oversight. Your kidney? It's a bargaining chip.