For millions of people, statins are a daily pill that keeps heart attacks and strokes at bay. But for others, that same pill brings aching legs, sore shoulders, or just a constant feeling of being worn out. If you’ve been prescribed a statin and are wondering whether the benefits are worth the discomfort, you’re not alone. The truth is, statins work - really well - but they don’t work the same for everyone. And muscle pain? That’s the biggest reason people stop taking them.
How Statins Actually Lower Cholesterol
Statins don’t just reduce cholesterol. They rewire how your liver handles it. These drugs block an enzyme called HMG-CoA reductase, which your liver uses to make cholesterol. When that enzyme slows down, your liver starts pulling more LDL - the bad kind - out of your blood to use as raw material. It’s like turning off the factory and opening the warehouse doors to pull in more stock from outside.
On average, a standard dose of a statin like atorvastatin or rosuvastatin cuts LDL cholesterol by 40 to 60%. That’s not a small drop. For someone with an LDL of 190 mg/dL, that could bring it down to 80 or 90 - a change that slashes heart attack risk by about 60%. The effect isn’t just about cholesterol numbers. Statins also calm inflammation in artery walls, stabilize plaque so it doesn’t rupture, and help the lining of blood vessels work better. That’s why even people with normal cholesterol but high heart disease risk still benefit.
Landmark studies like the Heart Protection Study and the 4S trial followed tens of thousands of people for years. The results were clear: those on statins had far fewer heart attacks, strokes, and deaths from heart disease. For people who’ve already had a heart attack, statins cut the chance of another one by nearly half. That’s why doctors keep prescribing them - the data doesn’t lie.
The Muscle Pain Problem
But then there’s the other side. Around 1 in 10 people on statins report muscle aches, weakness, or cramps. It’s not rare. It’s common. And it’s not always mild. Some people describe it like a constant deep ache in their thighs or calves, worse after walking or climbing stairs. Others get sudden, sharp cramps at night that wake them up.
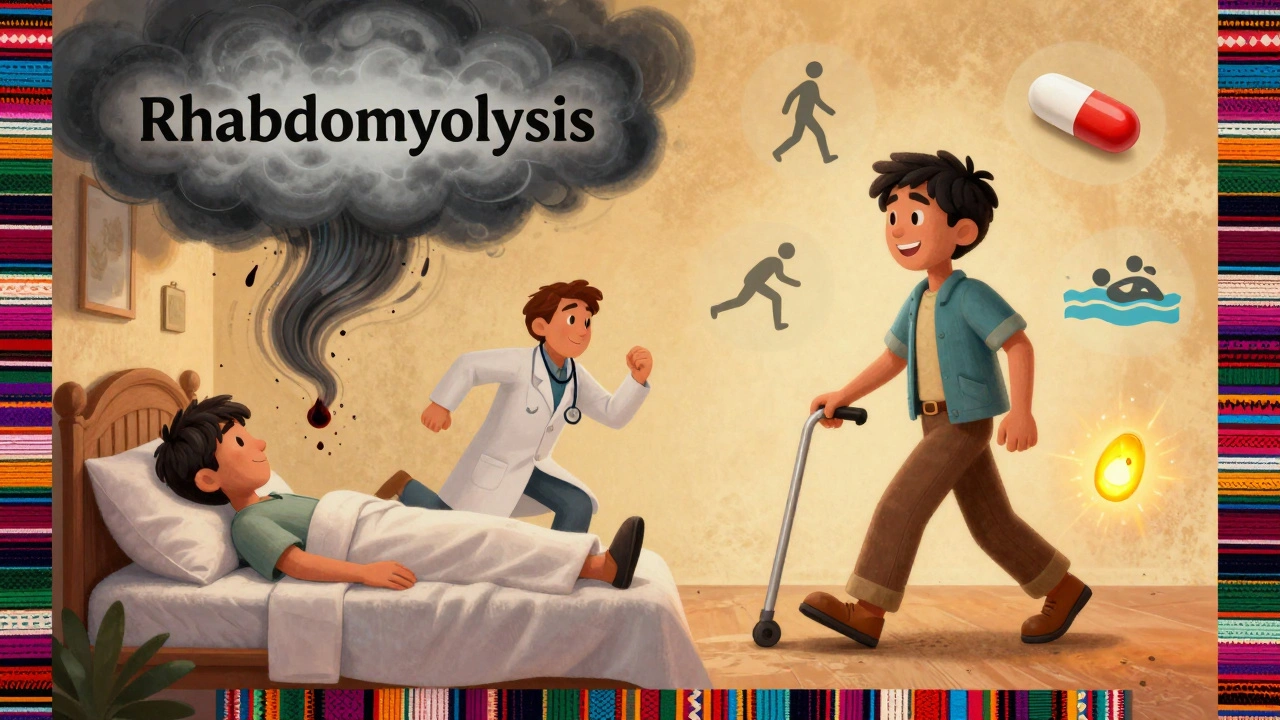
Here’s what most people don’t realize: this pain isn’t always from damage. In most cases, muscle enzymes like creatine kinase (CK) stay normal. That means the muscle isn’t breaking down - it’s just hurting. Doctors call this statin-associated muscle symptoms, or SAMS. It’s not rhabdomyolysis - that’s the rare, dangerous form where muscles literally start dying, with CK levels soaring. That happens in fewer than 1 in 1,000 people.
Why does it happen? Scientists aren’t 100% sure. One theory is that statins lower levels of coenzyme Q10, a compound your muscles need for energy. Another is that they interfere with how muscle cells handle calcium. Either way, the result is the same: tired, sore muscles that feel like they’ve been overworked - even if you haven’t exercised.
And here’s the catch: people often blame statins for muscle pain that’s actually from aging, arthritis, or just being less active. That’s why it’s so easy to misattribute. But if the pain started after you began the pill, and it gets better when you stop, that’s a strong clue.
Not All Statins Are the Same
If you’re having muscle pain, switching statins might help - a lot. Not all statins are created equal when it comes to side effects. Simvastatin and lovastatin are more likely to cause muscle issues, especially at higher doses. Atorvastatin and rosuvastatin are stronger and more commonly used now, but they can still cause problems. Pravastatin and fluvastatin, on the other hand, are less likely to trigger muscle pain. Why? They’re processed differently by the liver and don’t build up in muscle tissue as much.
One study found that 70% of patients who couldn’t tolerate simvastatin due to muscle pain were able to stay on pravastatin without issues. That’s not a small number. If you’re struggling, talk to your doctor about switching to a statin that’s gentler on muscles. Sometimes, just dropping the dose - say from 40 mg to 20 mg of atorvastatin - makes a big difference. You still get most of the heart protection, but with fewer side effects.
What Actually Helps With Muscle Pain
Coenzyme Q10 supplements are often suggested. Some people swear by them. The science? Mixed. A few small studies show a slight improvement in muscle symptoms. Others show no difference. It’s not a magic fix, but it’s low-risk. If you want to try it, 100-200 mg a day is a common dose.
Exercise might sound counterintuitive, but staying active helps. Gentle movement - walking, swimming, light resistance training - keeps muscles healthy and may reduce stiffness. Inactivity makes muscle pain worse. Don’t stop moving, even if it hurts a little.
Timing matters too. Some people find taking their statin at night helps, because cholesterol production peaks then. Others find taking it in the morning reduces muscle soreness during the day. It’s worth experimenting - under your doctor’s guidance.
And don’t ignore other triggers. Drinking grapefruit juice can boost statin levels in your blood and make muscle pain worse. Alcohol, certain antibiotics like clarithromycin, and even some supplements can interact. Always check with your pharmacist before adding anything new.
When to Stop - and When Not To
Here’s the hard truth: stopping statins because of muscle pain is one of the biggest mistakes people make. A 2014 study found that almost half of people quit within a year - and their heart attack risk went right back up. The pain is real, but the risk of a heart attack is far worse.
If you have mild muscle soreness, don’t quit. Work with your doctor. Try a different statin. Lower the dose. Add CoQ10. Give it a few weeks. Most people find a version that works.
But if you have severe pain, dark urine (a sign of muscle breakdown), or weakness so bad you can’t climb stairs, stop the medication and call your doctor immediately. That’s not normal. That’s a red flag.
The goal isn’t to suffer through pain. It’s to find a balance - enough protection, without too much discomfort. That balance looks different for everyone.
Who Should Be on Statins?
Statins aren’t for everyone. Guidelines say they’re recommended for:
- People who’ve had a heart attack, stroke, or angioplasty
- People with diabetes and high LDL (over 70 mg/dL)
- People with very high LDL (over 190 mg/dL)
- People with a 10-year heart disease risk over 7.5% (calculated using age, blood pressure, cholesterol, smoking status)
If you’re healthy, with normal cholesterol and no other risks, statins usually aren’t needed. But if you’re in one of those high-risk groups, the math is simple: the benefit is huge. The risk of muscle pain? Manageable.
And here’s something most people don’t know: even if you feel fine, statins are working. You won’t feel better - you’ll just not have a heart attack. That’s the invisible win.
The Bigger Picture
Statins are one of the most studied drugs in history. Over 100 million people have taken them. The evidence is overwhelming: they save lives. But they’re not perfect. Muscle pain is the trade-off for many. And it’s not something to ignore - but it’s also not a reason to give up on protection.
Today, doctors are getting better at personalizing statin therapy. Genetic tests can now spot people who are more likely to have muscle side effects from simvastatin. New formulations are being tested to target blood vessels without affecting muscles. For now, though, it’s about finding the right fit.
If you’re on a statin and having trouble, don’t assume it’s a dead end. Talk to your doctor. Try a different one. Adjust the dose. Give it time. The goal isn’t to be pill-free. It’s to live longer, healthier, and without a heart attack. And for most people, that’s still possible - even with muscle pain.
Do statins really lower the risk of heart attacks?
Yes. For every 1 mmol/L (39 mg/dL) drop in LDL cholesterol, major heart events like heart attacks and strokes drop by about 22%. In people with existing heart disease, statins cut the risk of another heart attack by nearly 50%. Studies with over 100,000 participants confirm this - the benefit is real and long-lasting.
Is muscle pain from statins dangerous?
Most of the time, no. Muscle aches without rising creatine kinase (CK) levels are called statin-associated muscle symptoms (SAMS). They’re uncomfortable but not harmful. True muscle damage - rhabdomyolysis - is extremely rare, affecting fewer than 1 in 1,000 users. Dark urine, extreme weakness, or fever are red flags that need immediate medical attention.
Can I switch to a different statin if I have muscle pain?
Absolutely. Not all statins cause the same side effects. Pravastatin and fluvastatin are less likely to trigger muscle pain than simvastatin or atorvastatin. Many people who can’t tolerate one statin do fine on another. Switching is often the first step before quitting entirely.
Does taking CoQ10 help with statin muscle pain?
Some people find relief, but the evidence isn’t strong. CoQ10 levels drop with statin use, and since it’s important for muscle energy, supplementing makes sense. Studies show mixed results - some report less pain, others see no change. It’s low-risk, so trying 100-200 mg daily is reasonable if you’re having symptoms.
Can I stop statins if I feel fine?
Only if your doctor agrees. Statins work silently - you won’t feel them working. Stopping means your LDL rises again, and your risk of heart attack climbs back to where it was before. For high-risk people, the protection is ongoing. Don’t stop just because you feel okay. Talk to your doctor first.
Are generic statins as good as brand names?
Yes. Generic atorvastatin, simvastatin, and rosuvastatin are chemically identical to their brand-name versions (Lipitor, Zocor, Crestor). They’re just cheaper - often under $4 a month. The FDA requires generics to work the same way. There’s no reason to pay more unless your doctor has a specific reason.
What to Do Next
If you’re on a statin and having muscle pain, don’t panic. Don’t quit. Do this:
- Write down when the pain started and what it feels like.
- Check if you’re taking grapefruit juice or other drugs that might interact.
- Ask your doctor about switching to pravastatin or lowering your dose.
- Try CoQ10 for 4-6 weeks - it won’t hurt.
- Keep moving. Even light walking helps.
If the pain is severe or you notice dark urine, stop the medication and call your doctor right away. But for most people, the solution isn’t stopping statins - it’s finding the right one. The heart protection is too important to give up without trying other options first.


Comments (8)
Gillian Watson
I’ve been on rosuvastatin for 5 years and never had a single muscle ache. But my cousin switched from simvastatin to pravastatin and said it was like night and day. Maybe it’s not the drug-it’s the match.
Also, grapefruit juice? Don’t even get me started.
Gareth Storer
So let me get this straight. You’re telling me the pharmaceutical industry spent billions to make a drug that makes people feel like they’ve been hit by a truck… so they don’t die of a heart attack? Brilliant. Absolute genius. I’m sure the CEO’s yacht is fully paid off.
Benjamin Sedler
Statins are just the latest corporate psyop to turn healthy people into pill-popping zombies. You think your LDL is ‘too high’? Nah. You’re just not eating enough saturated fat. Butter is medicine. Coconut oil is the real statin. The FDA’s been in bed with Big Pharma since Nixon. Look up the ‘Lipitor scandal’-it’s not a myth, it’s a dossier.
And CoQ10? That’s what they want you to take so you don’t notice the real problem: your liver’s been poisoned by glyphosate. Wake up.
Jessica Baydowicz
I was skeptical too-until I started walking my dog every morning after switching to pravastatin. The muscle fog lifted, and I actually started enjoying life again. Don’t give up on statins, just find your version. And yes, CoQ10 helped me. Not magic, but real.
You’re not weak for feeling this. You’re human. And you deserve to feel good while staying safe.
Pavan Kankala
They don’t tell you this but statins are basically chemical castration for your muscles. The real reason they work so well? They lower testosterone. That’s why old men on statins look like they’ve been drained by a vacuum. No muscle pain? Just low libido and zero energy. You think that’s worth it? Ask your doctor if they take it themselves. I bet they don’t.
Elizabeth Crutchfield
i started takin statins last year and my legs felt like cement. i tried coq10 and it helped a lil but honestly i just started walking more and now i barely notice it. also no grapefruit. ever. like, not even a slice. that stuff is evil.
John Filby
I switched from atorvastatin to fluvastatin last month and wow. The difference is insane. No more 3pm leg cramps. I was ready to quit, but my pharmacist suggested the switch. Honestly, pharmacists know more than doctors sometimes. Also, CoQ10 didn’t do much for me, but moving more did. Just 10 minutes a day. Life changed.
Also-yes, generics are fine. I pay $3 a month. No regrets.
Yasmine Hajar
I used to think muscle pain meant I was broken. Turns out, I just needed the right statin. Pravastatin saved me. I’m 62, have diabetes, and I’m still hiking. Statins aren’t the enemy. Giving up is. You don’t have to suffer-you just have to keep looking. Talk to your doc. Try one more time. You’re worth it.