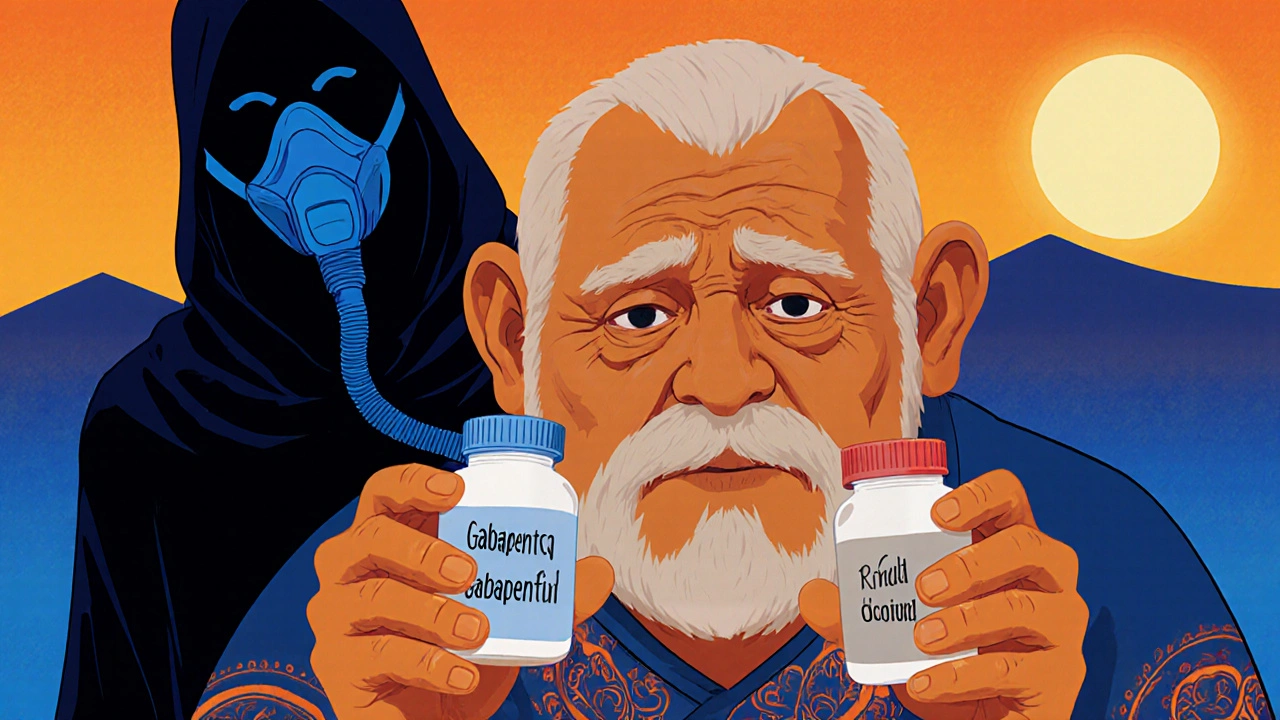
Gabapentinoids with Opioids: Risks, Real-World Use, and Safety Tips
When doctors prescribe gabapentinoids with opioids, a combination of nerve pain medications like gabapentin or pregabalin and opioid painkillers. Also known as neuropathic pain combos, it's often used for chronic pain that doesn’t respond to either drug alone. But this mix isn’t harmless—it’s one of the most dangerous pairings in modern pain management.
People often think if one pill helps, two must help more. But with gabapentin, a medication originally for seizures that’s now widely used for nerve pain and pregabalin, its stronger cousin, approved for fibromyalgia and diabetic nerve pain, adding opioids doesn’t just boost pain relief—it multiplies the risk of breathing problems, overdose, and death. Studies show patients on both drugs are up to four times more likely to die from respiratory failure than those on opioids alone. The FDA has warned about this since 2019, yet prescriptions keep rising, especially in older adults and those with long-term pain.
Why do doctors still prescribe this combo? Because for some, the pain is unbearable. A patient with spinal nerve damage or post-surgical neuropathy might get minimal relief from gabapentin alone, and opioids alone carry addiction risks. So they try both—thinking they’re being smart. But here’s the catch: gabapentinoids don’t just add to opioids—they change how your brain processes them. They make you drowsier, slower to react, and more likely to stop breathing while sleeping. Even small doses become risky when mixed.
You won’t find this combo in most guidelines as a first-line treatment. It’s a last-resort option, used only after safer drugs like antidepressants, physical therapy, or topical treatments have failed. And even then, it’s not a long-term solution. The longer you stay on both, the higher your tolerance climbs—and the more you need just to feel normal. That’s when dependence turns to addiction.
What should you do if you’re on this combo? Don’t stop suddenly. Talk to your doctor about tapering one drug at a time. Ask if non-opioid options like duloxetine or lidocaine patches could work. Check if your pain clinic offers nerve blocks or cognitive behavioral therapy. These aren’t quick fixes, but they’re far safer than living with the constant shadow of overdose.
The posts below show real cases where people managed pain without this risky combo—how one person switched from gabapentin and oxycodone to a spinal stimulator, how another found relief with acupuncture and exercise after years of opioids, and how pharmacies now flag dangerous combinations before filling prescriptions. You’ll also find guides on recognizing early signs of overdose, how to store these meds safely at home, and what to do if a loved one is using them. This isn’t about scare tactics. It’s about giving you the facts so you can make smarter choices—for your body, your family, and your future.