Inflammation and Osteoporosis Link
When talking about the inflammation osteoporosis link, the relationship between persistent inflammatory activity and reduced bone density. Also known as the inflammation‑induced bone loss pathway, it shows how long‑standing inflammation can accelerate osteoporotic changes.
Why Inflammation Matters for Bones
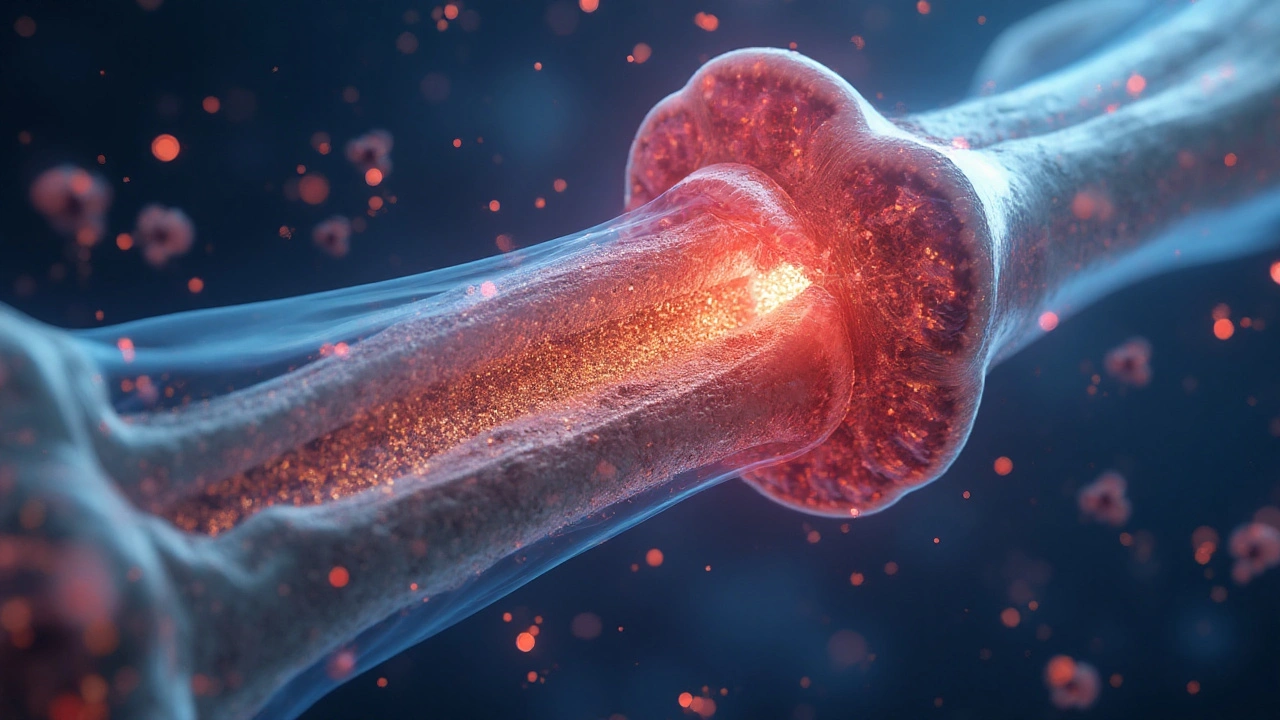
Inflammation, marked by swelling, heat, and immune cell activation, isn’t just a symptom of injury. Inflammation, a protective response that can become chronic when the trigger persists releases a flood of signaling proteins called cytokines. When these cytokines hang around, they start to interfere with the normal balance of bone formation and resorption. Think of it as a construction crew that never takes a break – the demolition crew (osteoclasts) keeps tearing down walls while the builders (osteoblasts) can’t keep up.
One of the biggest culprits is tumor‑necrosis factor‑alpha (TNF‑α). It tells osteoclasts to gear up, while simultaneously shutting down the activity of osteoblasts. That double‑hit means bone loss speeds up, especially in places like the spine and hip where osteoporosis typically shows up.
Osteoporosis, osteoporosis, a disease characterized by porous, fragile bones, traditionally gets linked to age, menopause, or calcium deficiency. Yet mounting evidence shows that chronic inflammation is a hidden driver, especially in conditions like rheumatoid arthritis, inflammatory bowel disease, and even long‑term obesity. The inflammation osteoporosis link isn’t just a theory – it’s observed in bone‑density scans of patients with persistent inflammatory disorders.
Understanding this connection helps clinicians decide when to screen for bone loss, even in younger patients who might otherwise be considered low‑risk. It also opens up treatment options that target the inflammatory cascade, not just the bone cells.
Cytokines and Bone Remodeling: The Molecular Bridge
Cytokines act as messengers between immune cells and bone cells. Cytokines, small proteins that regulate inflammation and immune responses such as interleukin‑1 (IL‑1), IL‑6, and RANKL (receptor activator of nuclear factor‑kappa B ligand) directly stimulate osteoclast differentiation. In a healthy system, bone remodeling is a balanced dance: osteoclasts break down old bone, osteoblasts lay down new matrix. When cytokines tip the scale, the choreography collapses, and bone loss dominates.
RANKL is a key player. It binds to its receptor RANK on osteoclast precursors, prompting them to mature and start resorbing bone. Inflammatory conditions often up‑regulate RANKL while down‑regulating its natural inhibitor, osteoprotegerin (OPG). The result? More aggressive bone erosion. Therapies that block RANKL, like denosumab, have shown success in both osteoporosis and inflammatory arthritis, illustrating how targeting the molecular bridge can mitigate the link.
Another cytokine, IL‑6, fuels the liver to produce C‑reactive protein (CRP), a systemic marker of inflammation. High CRP levels correlate with faster bone loss in longitudinal studies. So measuring CRP can give a snapshot of how active the inflammation‑osteoporosis pathway is in a given patient.
Medication Impacts: From Steroids to NSAIDs
Medications that either provoke or suppress inflammation can sway bone health dramatically. Long‑term glucocorticoids, while excellent at dampening inflammation, are notorious for accelerating bone loss. They reduce calcium absorption, increase urinary calcium loss, and directly impair osteoblast function. This paradox means that patients on steroids often need concurrent bone‑protective strategies, such as bisphosphonates or calcium‑vitamin D supplementation.
On the flip side, non‑steroidal anti‑inflammatory drugs (NSAIDs) may offer modest bone‑sparing effects by lowering prostaglandin‑mediated inflammation. However, not all NSAIDs are equal; some studies suggest selective COX‑2 inhibitors could impair bone healing, while traditional NSAIDs might be safer for long‑term use. The medication landscape covered in the articles below—ranging from antiplatelet agents to antidepressants—highlights how drug choices intersect with bone health, especially when inflammation is a factor.
Emerging biologics that target specific cytokines (e.g., anti‑TNF agents) have shown dual benefits: controlling disease activity and slowing bone erosion in rheumatoid arthritis. Yet these drugs are expensive and not universally accessible, underscoring the need for personalized risk assessments.
Lifestyle, Nutrition, and Exercise: Counteracting the Link
Even with the best medical care, lifestyle choices can tip the balance back toward bone formation. Weight‑bearing exercise—like walking, resistance training, or dancing—stimulates osteoblasts through mechanical loading. When inflammatory markers drop after regular activity, the cytokine surge that fuels bone loss also subsides.
Nutrition plays a complementary role. Adequate calcium and vitamin D are the building blocks for bone matrix, while omega‑3 fatty acids from fish oil have anti‑inflammatory properties that can lower cytokine levels. Some research links a Mediterranean‑style diet to higher bone mineral density, possibly because of its anti‑inflammatory profile.
Weight management matters, too. Excess adipose tissue secretes pro‑inflammatory adipokines like leptin and resistin, which can contribute to the inflammation‑osteoporosis axis. Losing weight in a controlled manner can reduce these signals and improve bone turnover markers.
What You’ll Find in This Collection
The articles below dive into specific meds, disease interactions, and practical tips that tie back to the inflammation osteoporosis link. Whether you’re curious about how a drug like doxepin might affect your ear health, or you want a safe guide to buying generic medications online, each post adds a piece to the puzzle of managing inflammation and protecting bone health. Browse through the list to see real‑world examples, detailed drug comparisons, and actionable advice that complements the science we’ve just covered.