TZD Side Effects Calculator
Input Your Details
Your Results
When you're managing type 2 diabetes, every medication comes with trade-offs. Thiazolidinediones, or TZDs - like pioglitazone (Actos) and rosiglitazone (Avandia) - are powerful at improving insulin sensitivity. But for many people, the benefits come with two big downsides: weight gain and fluid retention (edema). If you’ve noticed your ankles swelling, your clothes feeling tighter, or the scale jumping up without changes in diet or activity, you’re not alone. About 60% of people on TZDs gain weight, and up to 16% develop noticeable edema - especially when used with insulin.
Why TZDs Cause Weight Gain and Swelling
It’s not just about eating more. TZDs work by activating PPAR-γ receptors, which help your body use insulin better. But that same mechanism triggers fluid buildup. Around 65-70% of the weight gain you see isn’t fat - it’s extra water. Your kidneys start holding onto sodium, which pulls water into your bloodstream. This increases your blood volume, leading to swelling in your legs, feet, and sometimes hands. The swelling usually shows up early - within the first few weeks. Some people gain 2-5 kg in just a month. The problem gets worse if you’re also taking insulin. Together, they cause blood vessels to widen, which makes your kidneys hold even more fluid. It’s not just your legs, either. Fluid can build up in your lungs, which is why TZDs come with a black box warning from the FDA: don’t use them if you have moderate to severe heart failure (NYHA Class III or IV).Who Should Avoid TZDs Altogether
TZDs aren’t for everyone. If you already have heart failure, kidney disease, or a history of fluid buildup, your doctor should avoid prescribing them. The risk isn’t theoretical - in clinical trials, people with heart issues on TZDs were 2-3 times more likely to be hospitalized for heart failure than those on other drugs. Even if you don’t have heart failure, you need to be cautious if you’re older, have high blood pressure, or have had swelling before. Women are more likely to develop edema than men - possibly due to hormonal differences in how the kidneys respond. If you’re over 65, your doctor should start you on the lowest possible dose and watch you closely.How to Reduce Weight Gain and Swelling
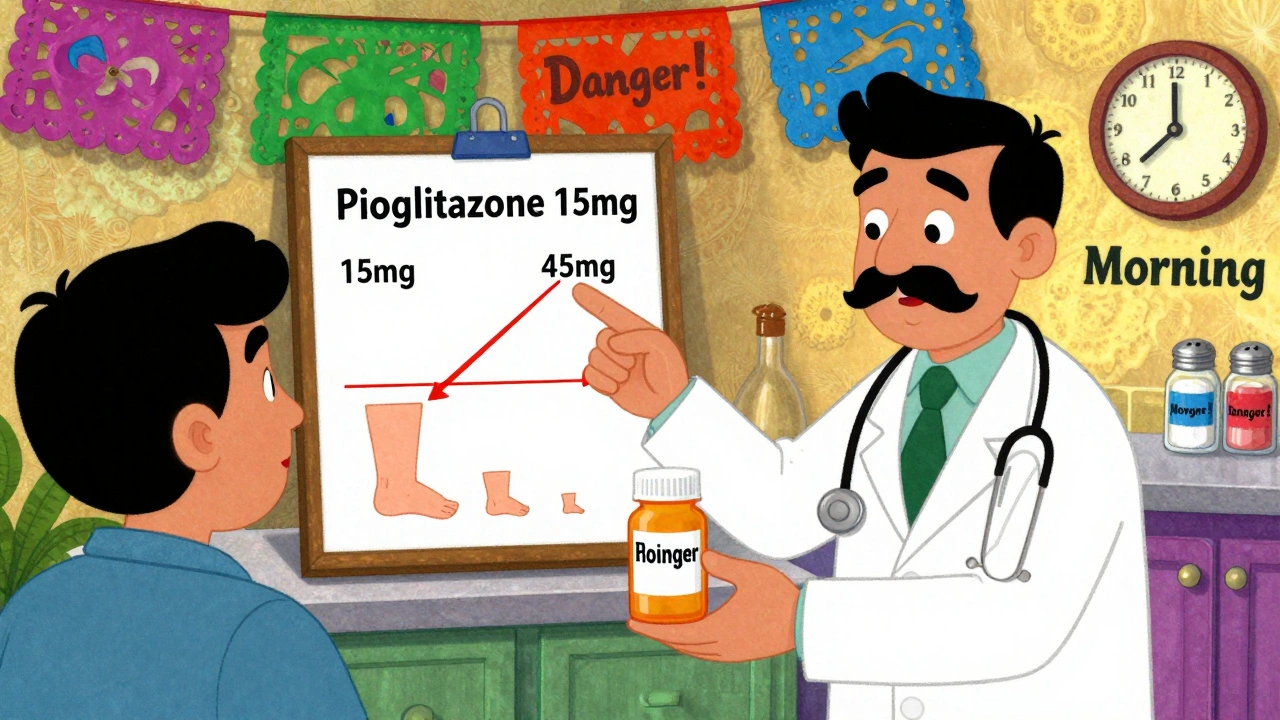
You don’t have to quit TZDs if you’re benefiting from them. Many people keep using them - but they manage the side effects. Here’s what actually works:- Start low, go slow. Pioglitazone at 15 mg daily causes only 2.1% edema. At 45 mg, it jumps to nearly 5%. Starting low cuts your risk in half.
- Take it in the morning. Fluid retention tends to worsen at night. Taking your pill in the morning gives your body time to process it before you lie down.
- Watch your salt. Limit sodium to under 2,000 mg per day. That means no processed foods, canned soups, or salty snacks. Read labels. Even one bag of chips can push you over.
- Elevate your legs. If your ankles swell, prop them up for 15-20 minutes a few times a day. It helps drain the fluid back toward your heart.
- Track your weight daily. Weigh yourself at the same time each morning, after using the bathroom, in light clothing. If you gain more than 2-3 kg in a week, call your doctor. Early action can prevent hospitalization.
Combination Therapy: The Smart Way to Use TZDs
The most effective strategy for reducing edema isn’t just lifestyle - it’s pairing TZDs with the right other meds. SGLT2 inhibitors - like empagliflozin (Jardiance) or dapagliflozin (Farxiga) - are game-changers. These drugs make your kidneys flush out sugar and sodium. When combined with a TZD, they cut fluid retention by up to 45%. That’s not just a number - it means fewer swollen ankles, less shortness of breath, and less risk of heart failure hospitalization. Some doctors also use low-dose thiazide diuretics - like hydrochlorothiazide - to help with swelling. But avoid loop diuretics (like furosemide) unless absolutely necessary. They can mess with your electrolytes and make blood sugar harder to control.What Doesn’t Work
Don’t waste time on things that sound right but don’t help:- Crash diets. Losing weight fast won’t fix fluid retention - and may make your blood sugar unstable.
- Herbal diuretics. Dandelion, green tea, or hibiscus tea might seem natural, but they’re not strong enough and can interact with your meds.
- Skipping doses. Stopping your TZD suddenly can cause your blood sugar to spike. Always talk to your doctor first.

When to Consider Stopping TZDs
If you’re gaining weight, swelling gets worse, or you feel short of breath - especially when lying down - it’s time to talk to your doctor. You might need to switch. Newer drugs like GLP-1 agonists (semaglutide, liraglutide) and SGLT2 inhibitors not only help blood sugar - they often cause weight loss and reduce heart risks. TZDs are no longer first-line. The American Diabetes Association now recommends them only after metformin and newer agents have been tried. But they still have a place - especially for people with severe insulin resistance who haven’t responded to anything else. The key is using them smartly.What’s Next for TZDs
Scientists are working on next-generation drugs that keep the insulin-sensitizing benefits of TZDs but avoid the fluid retention. Early versions, like saroglitazar, show promise - with 60% less edema in trials. There’s also research into genetic testing. Some people have a gene variant (rs1801282) that makes them way more likely to retain fluid on TZDs. In the future, a simple blood test might tell you if this drug is right for you. For now, the message is clear: TZDs can work - but they demand attention. If you’re on one, don’t ignore the swelling. Don’t downplay the weight gain. Track your numbers. Talk to your doctor. With the right approach, you can keep the benefits without the burden.Does pioglitazone cause more weight gain than rosiglitazone?
No, both cause similar amounts of weight gain - around 2.7 to 3.0 kg on average. Rosiglitazone has a slightly higher risk of heart-related issues, which is why it’s rarely used today. Pioglitazone is the preferred TZD because it has a better safety profile, especially for the heart, even though the weight gain and swelling are about the same.
Can I lose the weight gained from TZDs?
The water weight usually goes down if you reduce your dose, cut salt, or add an SGLT2 inhibitor. The fat gain is harder to reverse and requires diet and movement. But many people find that once the fluid drops, they’re more motivated to make lifestyle changes - and then the fat follows.
Is edema from TZDs dangerous?
Mild swelling in the ankles is common and usually not dangerous. But if it spreads to your abdomen, you feel short of breath, or you gain more than 2-3 kg in a week, it could be a sign of heart failure. That’s a medical emergency. Always report rapid weight gain or breathing problems to your doctor right away.
How long does it take for TZD swelling to go away after stopping?
Most people see improvement in swelling within 1-2 weeks after stopping TZDs. Full resolution can take up to 4-6 weeks, depending on how long you were on the drug and how much fluid you retained. Combining it with sodium restriction and leg elevation speeds up recovery.
Can I take a diuretic with TZDs to reduce swelling?
Yes - but only under medical supervision. Thiazide diuretics like hydrochlorothiazide are preferred because they’re mild and don’t interfere much with blood sugar. Loop diuretics (like furosemide) are stronger but can cause low potassium and make blood sugar harder to control. Never start a diuretic on your own.
Are there any natural ways to reduce TZD-related swelling?
The most effective natural strategies are reducing sodium intake, elevating your legs, and staying active with light walking. Avoid alcohol and tight clothing. Herbal remedies like dandelion or parsley aren’t proven to help and may interact with your diabetes meds. Stick to evidence-based methods - they’re safer and more reliable.


Comments (9)
pallavi khushwani
Been on pioglitazone for two years. The swelling was brutal at first-felt like I was walking with concrete boots. Started cutting salt, lifted my legs after work, and switched to morning doses. Big difference. Also added Jardiance last year and the edema cut in half. No magic, just smart tweaks.
Shayne Smith
I love how this post doesn’t just say ‘stop the drug’ but gives real tools. So many docs just shrug and say ‘it’s a side effect’ like it’s inevitable. Not cool. This is what patient education should look like.
Geraldine Trainer-Cooper
the whole tzd thing is just capitalism in pill form. they keep selling us drugs that make us gain weight so we need more drugs to fix the side effects. it’s a loop. we’re all lab rats. no one’s talking about the real problem: why we even need these drugs in the first place.
olive ashley
Did you know the FDA’s black box warning was buried in a 400-page document nobody reads? And the drug companies funded 80% of the ‘safe use’ studies? I’ve seen patients with stage 3 heart failure still on pioglitazone because their doctor ‘didn’t realize.’ It’s not negligence-it’s systematic. Wake up.
Ibrahim Yakubu
Back home in Nigeria, we don’t even have access to these fancy SGLT2 inhibitors. We get metformin and sometimes pioglitazone if we’re lucky. And yes, people swell. But we elevate legs, drink bitter leaf tea, and walk barefoot on grass. Sometimes traditional wisdom beats pharmaceutical hype.
Andrew Frazier
fr tho why are women so much more likely to swell? is it just their bodies being weak or what? like i get it they got hormones but come on. if you can’t handle a little water weight maybe you shouldn’t be on meds. #manup
Karen Mitchell
It is profoundly irresponsible to suggest that dietary sodium reduction alone can mitigate pharmacologically induced fluid retention. This is not a lifestyle issue-it is a pharmacokinetic one. The suggestion that one can ‘manage’ this with leg elevation borders on dangerous misinformation. Patients require physician-guided intervention, not folk remedies.
Nava Jothy
I’ve been on this drug for 5 years and I’ve gained 30lbs. My ankles look like balloons. My husband says I cry too much. But I’m alive. And my HbA1c is 5.8. So who’s the real villain here? The drug? Or the system that gave me no other choice? 😭💔
Mansi Bansal
While the clinical data presented is methodologically sound, one must interrogate the underlying epistemological framework that privileges pharmaceutical intervention over systemic metabolic reconfiguration. The normalization of TZD use reflects a biomedical hegemony that pathologizes insulin resistance as a condition to be medicated, rather than a signal of dietary and environmental dysregulation. One cannot pharmacologically compensate for a society that commodifies glucose.