Switching from brand-name warfarin (Coumadin) to a generic version might seem like a simple cost-saving move-but for patients on this medication, it’s not that simple. Warfarin isn’t like taking a generic painkiller. It’s a warfarin that demands precision. Too little, and you risk a stroke or blood clot. Too much, and you could bleed internally. That’s why every switch, even to a generic that’s supposed to be "therapeutically equivalent," needs careful attention.
Why Warfarin Is Different
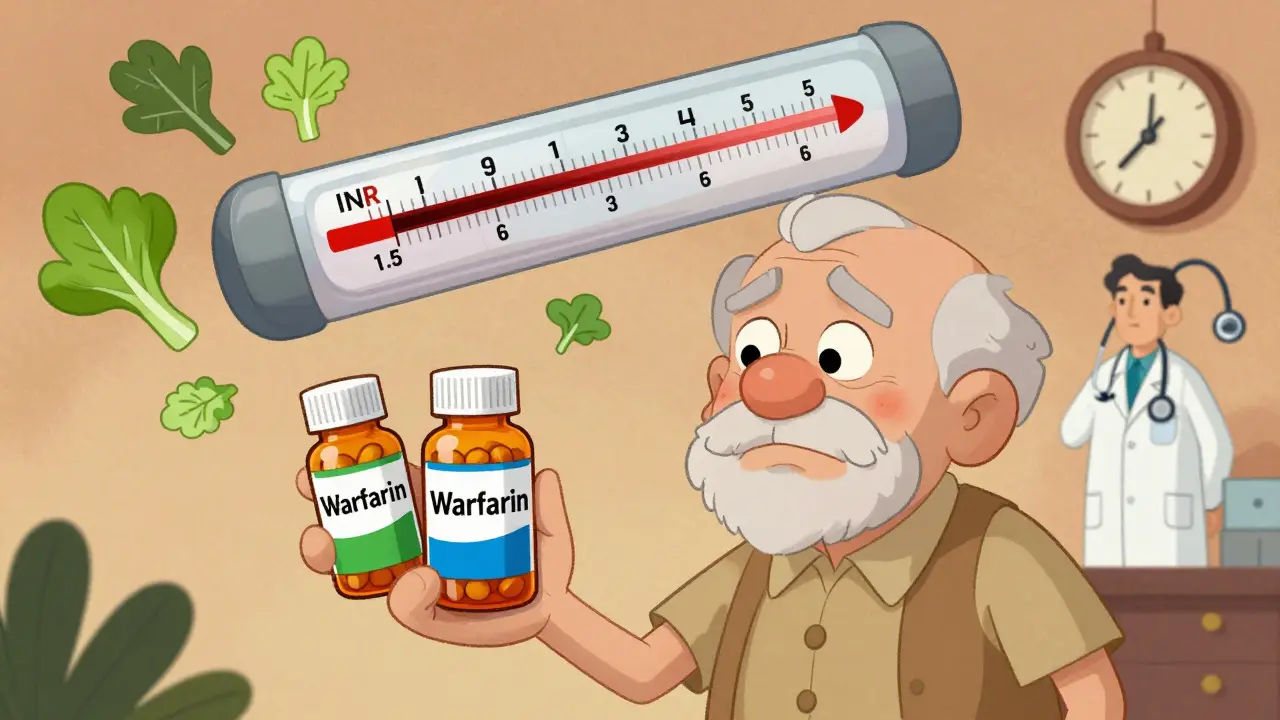
Warfarin has been around since the 1950s. It’s one of the oldest blood thinners still in wide use. Unlike newer drugs like apixaban or rivaroxaban, warfarin doesn’t come with a fixed dose. Its effect changes from person to person-and even from one batch of pills to another. That’s because it’s a narrow therapeutic index drug. The difference between a safe dose and a dangerous one is tiny. For most people, the target INR (International Normalized Ratio) is between 2.0 and 3.0. That’s a very small window. If your INR drops to 1.5, you’re at risk for clots. If it climbs to 4.5, you’re at risk for bleeding.
Why does this matter for generics? Because even small changes in how the drug is absorbed can push your INR out of range. Generic warfarin must prove it’s "bioequivalent" to Coumadin-meaning it delivers 80% to 125% of the same amount of drug into your bloodstream. Sounds fine, right? But for warfarin, that 45% range is wide enough to cause trouble. One study found that switching between different generic brands caused INR fluctuations in 15-20% of patients. Not everyone. But enough to be dangerous.
What Happens When You Switch Generics?
Most patients switch without issues. In fact, over 80% of people who move from Coumadin to a generic warfarin don’t have any major INR changes. But the other 15-20%? Their numbers go up or down unpredictably. Why? Because even though the active ingredient is the same, the inactive ingredients-fillers, binders, coatings-can vary between manufacturers. These don’t affect most drugs, but with warfarin, they can change how fast the pill dissolves in your gut. And that changes how much drug gets into your blood.
One real-world example: a 72-year-old woman in Perth was stable on Coumadin for five years. Her INR stayed at 2.6. Her doctor switched her to a generic made by Teva. Within ten days, her INR jumped to 4.2. She didn’t have symptoms, but her doctor ordered a CT scan just in case. Nothing showed up. But her dose had to be cut by 25%, and she needed weekly INR checks for a month before things settled. That’s not rare. That’s predictable.
That’s why experts agree: if you’re switching from one warfarin product to another-whether brand to generic or generic to generic-you need more frequent monitoring. Not every few weeks. Not every month. You need checks every 2-3 days for the first week, then weekly for the next two weeks. That’s the standard recommended by the Cleveland Clinic and the American Family Physician journal. It’s not overkill. It’s necessary.
What Your Doctor Should Do
A good anticoagulation clinic won’t just swap your prescription and call it a day. They’ll ask:
- What brand were you on before?
- What generic are you switching to? (Not just "warfarin"-the manufacturer matters.)
- When was your last INR? What was the result?
- Have you changed your diet? Started a new vitamin? Taken antibiotics recently?
Because warfarin doesn’t just interact with other drugs-it interacts with food. A big bowl of spinach, kale, or broccoli can drop your INR. A sudden lack of vitamin K can make it spike. If you’ve been eating the same way for years and suddenly switch warfarin brands, your body’s response can be unpredictable.
Doctors also need to check for drug interactions. Warfarin clashes with over 300 medications. Antibiotics, antifungals, even some herbal supplements like St. John’s Wort can throw your INR off. A single dose of ciprofloxacin can push your INR into the danger zone within 72 hours. That’s why your pharmacist should be involved too. Many pharmacies now flag warfarin switches automatically.

When to Be Extra Careful
Some people are at higher risk when switching:
- Those with mechanical heart valves (target INR 2.5-3.5 or even 3.0-4.0)
- Patients with liver disease (warfarin is broken down in the liver)
- Older adults (especially over 75)
- People with a history of bleeding or clots
- Those who’ve had trouble controlling INR in the past
For these patients, switching generics isn’t just a risk-it’s a red flag. Many specialists avoid switching them at all. If they’re stable on Coumadin, they stay on it. If they’re on a generic and doing well, they don’t switch again. The goal isn’t cost savings. It’s safety.
How to Monitor Yourself
You don’t have to wait for your doctor to tell you to check your INR. If you’re on warfarin, you should know your numbers. Keep a log. Write down your INR, your dose, and what you ate the day before. If you notice:
- Your INR changed by more than 0.5 without a clear reason
- You’re bruising more easily
- You have dark stools, nosebleeds, or headaches
Call your clinic. Don’t wait. A small INR shift can become a life-threatening bleed in hours.
Also, never refill your warfarin from a different pharmacy without checking the label. One patient in Melbourne switched pharmacies and got a different generic. She didn’t notice the change. Her INR jumped from 2.8 to 4.1. She ended up in the ER with a brain bleed. It was preventable.

Warfarin vs. DOACs: The Real Choice
It’s easy to think newer blood thinners like Eliquis or Xarelto are better. And for many people, they are. They don’t need regular blood tests. They have fewer food interactions. But they cost 30-50 times more. In Australia, generic warfarin costs about $10 a month. DOACs? $300-$500. For people on fixed incomes, that’s not a choice-it’s a necessity.
Plus, warfarin can be reversed. If you have a major bleed or need emergency surgery, doctors can give you vitamin K or fresh frozen plasma to stop the bleeding. DOACs? Not always. Some reversal agents exist, but they’re expensive and not always available.
So while DOACs are great for many, warfarin still has a place. Especially for people with mechanical heart valves, severe kidney disease, or those who can’t afford the alternatives.
What You Should Do Today
If you’re on warfarin, here’s what to do:
- Check your prescription label. Know the manufacturer. Write it down.
- If your pharmacy switches your brand, ask: "Is this the same one I had before?" If not, request your old brand-or ask for more frequent INR checks.
- Get your INR checked within 3-5 days after any switch.
- Keep your diet consistent. Don’t suddenly start eating a lot of leafy greens.
- Tell every doctor and pharmacist you see that you’re on warfarin.
- Keep a log of your INR results, doses, and any symptoms.
Warfarin isn’t going away. It’s cheap. It’s effective. And for millions of people, it’s the only option. But it demands respect. Switching generics isn’t a trivial change. It’s a medical event. Treat it like one.
Can I switch between different generic warfarin brands safely?
Switching between different generic warfarin brands can cause INR changes in some patients-even if both are labeled "therapeutically equivalent." The FDA considers them interchangeable, but real-world data shows about 15-20% of patients experience fluctuations. Always get your INR checked 3-5 days after switching, and more frequently for the next two weeks. If you’re on warfarin for a mechanical valve or have had unstable INR before, avoid switching unless absolutely necessary.
How often should INR be checked after switching to a generic?
After switching from brand-name Coumadin to a generic-or between generics-INR should be checked every 2-3 days for the first week, then weekly for the next two weeks. Once your INR is stable for two consecutive checks, you can return to your regular schedule (usually every 4-6 weeks). But don’t assume stability. Always follow your doctor’s advice.
Why do some people have trouble with generic warfarin but not others?
It depends on genetics, diet, liver function, and other medications. Some people metabolize warfarin slowly due to CYP2C9 gene variants, making them extra sensitive to small changes in dose or absorption. Others have fluctuating vitamin K intake from diet. Older adults and those with liver disease are also more vulnerable. That’s why a one-size-fits-all approach doesn’t work. Monitoring is personal.
Should I avoid generic warfarin altogether?
No. For most people, generic warfarin is safe and effective. Over 90% of warfarin prescriptions in the U.S. are generic, and most patients do fine. The key is not avoiding generics-it’s managing the transition. If you’re stable on brand-name Coumadin, you may not need to switch. But if cost is an issue, generics are fine-with proper monitoring. Don’t refuse generics out of fear. Ask for better monitoring instead.
What should I do if my INR changes after switching?
If your INR changes by more than 0.5 without a clear cause (like a new medication or diet change), contact your doctor immediately. Don’t adjust your dose yourself. Your provider may need to repeat the test, check for drug interactions, or temporarily increase monitoring. In most cases, a small dose adjustment (5-10%) will bring you back into range. But ignoring it can lead to serious bleeding or clotting.
Final Thought
Warfarin isn’t outdated. It’s essential. And for many, it’s the only affordable way to prevent strokes and clots. But it’s not a drug you can treat like any other. Every switch, every change, every dose adjustment needs attention. Your life depends on it. Don’t assume it’s fine. Check your numbers. Ask questions. Stay in control. Because with warfarin, safety isn’t automatic-it’s earned.

Comments (14)
John Sonnenberg
Switching warfarin generics is like playing Russian roulette with your blood. One day you're fine, next day you're bleeding internally and your doctor says "it's probably just the new brand." No. It's not "probably." It's predictable. I've seen three people end up in the ER because their INR spiked after a pharmacy switch. No one warned them. No one asked if they'd changed pills. Just assumed "bioequivalent" meant "safe." It didn't. It never does.
Jessica Klaar
I’m a nurse in a rural clinic, and I see this every single week. A patient comes in with a bruise the size of a baseball, says they’ve been fine for months, then we check their INR-4.7. They switched from Mylan to Teva last month. We didn’t even know. The pharmacy didn’t notify us. The doctor didn’t ask. Patients think generics are interchangeable like aspirin. They’re not. We’ve started requiring a signed form before any warfarin switch now. It’s a pain, but it saves lives.
PAUL MCQUEEN
Look, I get it. Warfarin is finicky. But the whole "switching is dangerous" thing feels overblown. Most studies show 80%+ of patients have zero issues. The 15-20% who do? They’re the same people who panic every time their cat sneezes. You don’t need a CT scan every time your INR moves 0.3. Just monitor. Adjust. Breathe. The fearmongering here is doing more harm than the generics themselves.
glenn mendoza
It is with profound respect for the clinical complexity of anticoagulant management that I offer this perspective: the pharmacokinetic variability inherent in generic warfarin formulations is not merely a theoretical concern-it is a well-documented, empirically validated clinical phenomenon. The FDA’s bioequivalence threshold of 80–125% AUC is statistically acceptable for most medications, yet for drugs with a narrow therapeutic index, such as warfarin, this margin constitutes a clinically significant deviation. Therefore, the recommendation for intensified INR monitoring following any formulation change is not merely prudent-it is ethically imperative.
Kathryn Lenn
Let’s be real. Who benefits from this "switch to generic" nonsense? Big Pharma. They make the brand. Then they make the generic. Then they buy the pharmacies that switch you without telling you. The FDA? They’re on payroll. The doctors? They’re paid per visit, not per outcome. So you get a new bottle. Same pill. Different logo. You don’t even get a heads-up. And if you die? Well, at least they saved $12 a month. This isn’t medicine. It’s a Ponzi scheme with blood.
Chima Ifeanyi
The entire paradigm of bioequivalence is a neoliberal construct designed to commodify pharmacological equivalence under the guise of cost-efficiency. The pharmacodynamic variance in CYP2C9 substrates, compounded by epigenetic modulation of vitamin K metabolism, renders the current FDA thresholds statistically inadequate for precision medicine applications. A 45% bioavailability window is not equivalence-it is pharmacological roulette, and the systemic failure to mandate real-time pharmacogenomic screening before switching constitutes a structural violence against marginalized populations with limited healthcare access.
Tori Thenazi
Did you know that the FDA doesn’t require manufacturers to test generic warfarin against the original Coumadin batch? They test it against another generic. So if Teva switches to Mylan, and Mylan switches to SunPharma, and SunPharma switches to… you get the idea? It’s like a game of telephone. Your INR isn’t changing because of diet or stress. It’s changing because no one knows what’s in your pill anymore. And no one’s accountable. I’ve been on warfarin for 12 years. I’ve had 4 different generics. I keep a spreadsheet. I’m not paranoid. I’m informed.
Angie Datuin
I switched from Coumadin to a generic last year. No issues. INR stayed perfect. I’m not saying everyone’s fine. But I’m also not scared. Maybe it’s because I eat the same food every day. Maybe I’m just lucky. But I think the fear is bigger than the risk. I’d rather take the generic and save $300 a month than pay for brand and stress over it.
Camille Hall
If you’re on warfarin, you’re not just a patient-you’re a partner in your own care. That means knowing your numbers, asking questions, and speaking up when something feels off. You don’t need to be a doctor. You just need to be informed. And if your pharmacist doesn’t explain the switch? Find one who does. Your life is worth that extra 10 minutes of conversation.
Ashlyn Ellison
My grandma died from a brain bleed after a generic switch. They didn’t even tell us they changed the brand. Just gave her a new bottle. She didn’t know. We didn’t know. Now I check every pill. I write down the logo. I call the pharmacy. I don’t care if I sound crazy. I’d rather be annoying than bury someone else.
Jonah Mann
so i switched to generic warfarin and my inr went nuts. like 2.1 to 4.0 in 3 days. i thought i was just stressed. turned out the pharmacy gave me a different maker. i had to go to the er. now i take a pic of the pill every time i get it. and i call the pharmacy if it looks different. they think i’m weird. i don’t care. i’m alive. you should too.
Frank Baumann
I’m not just talking about warfarin. I’m talking about the entire system. You think your doctor cares? They’re paid by the hour. They don’t have time to explain why a pill with a different color stripe could kill you. You think your pharmacist cares? They’re under pressure to fill 80 prescriptions an hour. You think the FDA cares? They approved the generic because the math "looked good" on paper. But real people? Real bodies? They don’t fit in a spreadsheet. I’ve sat in waiting rooms with people who’ve bled out because no one told them to check their INR after a switch. This isn’t a medical issue. It’s a moral failure.
Scott Conner
wait so if i switch from one generic to another do i need to check my inr again? like even if i’ve been on generics for years? i thought once you’re on it you’re good? or is every switch a new risk? i’m confused. my doc just says "keep taking it" but now i’m scared.
Alex Ogle
I’ve been on warfarin for 18 years. I’ve been on five different generics. I’ve had two INR spikes. Both happened after pharmacy switches. Both were caught because I kept a log. I write down the manufacturer, the pill color, the lot number. I know my INR like I know my birthday. I don’t trust the system. I trust my notes. If you’re on warfarin, start a notebook. Don’t wait for a crisis. Write it down. Every time. Because when your life depends on a number, you don’t get a second chance.