Sulfonamide Medication Safety Checker
What do you know about your reaction?
Why This Matters
According to recent studies, 99.2% of people with mild reactions can safely take non-antibiotic sulfonamides. The FDA now requires labels on these drugs to specify "This product does not contain the structural elements associated with sulfonamide antibiotic allergies."
More than 1 in 10 people say they’re allergic to sulfa drugs. But here’s the truth: sulfonamide allergy is often mislabeled. Most of the time, it’s not a real allergy at all. It’s a rash that showed up a week after taking an antibiotic, a stomachache, or a headache that had nothing to do with your immune system. And because of that, millions of people are being denied safe, effective medications - not because they’re at risk, but because of outdated assumptions.
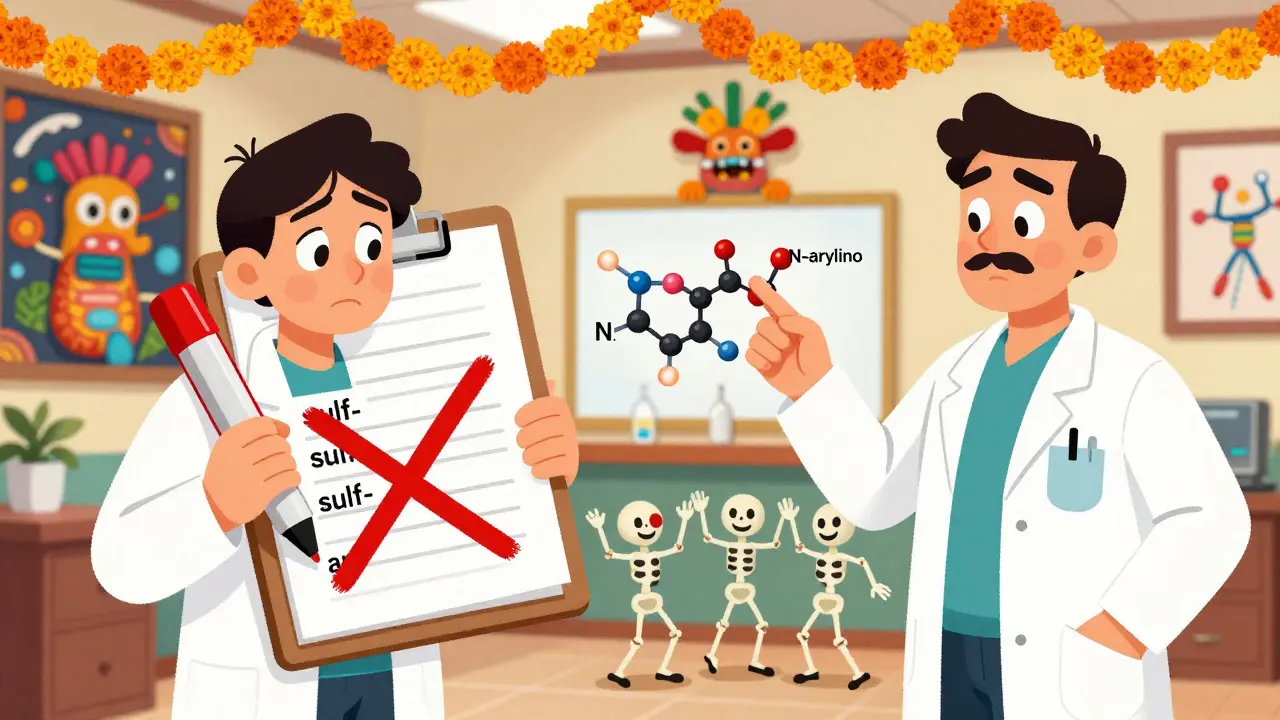
What’s Actually in a Sulfa Allergy?
When someone says they have a "sulfa allergy," they’re usually talking about a reaction to sulfonamide antibiotics - drugs like sulfamethoxazole (in Bactrim), sulfadiazine, or sulfacetamide. These were among the first antibiotics ever made, introduced in the 1930s. They work by blocking bacteria from making folic acid. But they also have a specific chemical structure: an arylamine group attached at the N4 position and a ring at N1. That’s what makes them potentially allergenic. The problem? The word "sulfa" gets thrown around like it’s one big danger zone. People think if they reacted to one sulfa drug, they can’t take anything with "sulf" in the name. That’s wrong. Sulfur, sulfates, and sulfites? Totally different chemicals. You can safely take Epsom salts (magnesium sulfate), insulin with preservatives (sulfites), or even diuretics like furosemide - even if you’ve had a reaction to Bactrim.Why Cross-Reactivity Is a Myth (Mostly)
Let’s clear up the biggest confusion: sulfonamide antibiotics do NOT cross-react with most other sulfonamide-containing drugs. That’s not just a guess - it’s backed by data from over 10,000 patients studied over the last decade. Take hydrochlorothiazide, a common blood pressure pill. It has the SO2NH2 group - the same basic building block - but no arylamine. That means it doesn’t trigger the same immune response. A 2020 study in the Journal of Allergy and Clinical Immunology found that patients with a documented sulfonamide antibiotic allergy had a 1.1% chance of reacting to hydrochlorothiazide. The control group without any sulfa history? 0.9%. No difference. Statistically, it’s noise. Same goes for celecoxib (Celebrex), acetazolamide (Diamox), and furosemide (Lasix). These are nonantimicrobial sulfonamides. They’re used for pain, glaucoma, seizures, and fluid retention. None of them share the exact structure that causes allergic reactions to antibiotics. The FDA now requires labels on these drugs to say: "This product does not contain the structural elements associated with sulfonamide antibiotic allergies."What You Should Actually Avoid
There are exceptions. If you’ve had a severe reaction - like Stevens-Johnson syndrome, toxic epidermal necrolysis, or anaphylaxis - to a sulfonamide antibiotic, you should avoid drugs with similar chemistry. That includes:- Dapsone (used for leprosy and Pneumocystis pneumonia prevention)
- Sulfasalazine (used for ulcerative colitis and rheumatoid arthritis)
- Sulfadiazine and sulfamethoxazole (the antibiotics you reacted to)
The Hidden Cost of Mislabeling
When a patient is labeled "sulfa allergic," doctors reach for alternatives. Vancomycin. Fluoroquinolones like ciprofloxacin. These drugs are broader-spectrum, more expensive, and carry serious risks: tendon rupture, aortic aneurysm, and C. diff infections. A 2021 study found that patients with a "sulfa allergy" label were 78% more likely to get a different antibiotic - and 33% of those were unnecessary broad-spectrum choices. That’s not just bad for the patient. It’s bad for everyone. Misuse of antibiotics drives resistance. The CDC reports that inappropriate antibiotic choices due to false sulfa allergy labels increase resistance rates in common bacteria like E. coli by 8.3% and Staphylococcus aureus by 12.7%. And the financial cost? Over $1.2 billion a year in the U.S. alone - extra hospital stays, more expensive drugs, longer recovery times.What to Do If You Think You Have a Sulfa Allergy
If you’ve been told you’re allergic to sulfa drugs, ask yourself: What actually happened?- Did you get a rash 5 days after starting the antibiotic? That’s common - and usually not allergic.
- Did you have hives, swelling, or trouble breathing within an hour? That’s a true IgE-mediated reaction - rare, but real.
- Did you feel nauseous or get a headache? That’s a side effect, not an allergy.
How to Talk to Your Doctor
Don’t just say, "I’m allergic to sulfa." Be specific. Write down:- Which drug you took (e.g., sulfamethoxazole-trimethoprim)
- What happened (e.g., "mild rash on day 4, no fever or swelling")
- When it happened (e.g., "4 days after starting")
- How it was treated (e.g., "stopped the drug, took Benadryl")

What About Sulfur, Sulfates, and Sulfites?
This myth won’t die. People think if they’re allergic to sulfa, they can’t take Epsom salts, IV contrast, or wine. Nope.- Sulfur is an element. It’s in your skin, hair, and joints. You can’t be allergic to it.
- Sulfates (like magnesium sulfate or sodium sulfate) are salts. Used in laxatives, Epsom baths, and IV fluids. No cross-reactivity.
- Sulfites are preservatives in wine and dried fruit. They can trigger asthma in sensitive people - but that’s a different mechanism entirely.


Comments (8)
Jason Jasper
I used to avoid all sulfa drugs after a rash in college. Turns out it was just a delayed side effect. Got tested last year with hydrochlorothiazide and had zero reaction. Feels good to finally take blood pressure meds without fear.
Thanks for the clarity.
Justin James
Let me tell you something the pharmaceutical industry doesn’t want you to know - this whole ‘sulfa allergy’ thing is a distraction. They’ve been pushing non-sulfa antibiotics for decades because they’re more profitable. Vancomycin? 10x the cost. Fluoroquinolones? Patent-protected monopolies. Meanwhile, sulfamethoxazole costs 12 cents a pill. And now they’re rebranding the fear with ‘SULF-RISK’ like it’s some breakthrough algorithm? Please. It’s just a rebrand. The same companies that sold you the drug that gave you the rash are now selling you the ‘safe’ alternative. Wake up. They’re not fixing your allergy - they’re fixing their profit margins. And don’t get me started on how EHR systems are coded to over-flag allergies so hospitals don’t get sued. It’s not medicine. It’s liability insurance dressed in white coats.
Lindsay Hensel
This is one of the most important pieces of medical misinformation I’ve ever seen corrected.
Thank you for writing this with such care and precision.
sagar patel
Proper labeling saves lives. Misclassification leads to inappropriate antibiotic use. Data is clear. No emotional speculation needed. Just facts.
Document your reaction. Be specific. Do not rely on vague terms. Medical records are not opinions. They are evidence.
Michael Dillon
Wait so you’re telling me I’ve been avoiding Celebrex for 15 years because I got a rash from Bactrim in 2009 and that was a mistake? Dude. I’ve been in pain because of this. I could’ve been hiking instead of on NSAIDs that wreck my stomach. This is insane. Why didn’t anyone tell me this before? I’m telling my entire family. This is wild.
Also - sulfur in wine? I thought that’s why I got headaches. Nope. Just wine. Thanks for that one too.
Gary Hartung
Oh, of course - because nothing says ‘evidence-based medicine’ like a 2020 study cited in a blog-style post with no peer-reviewed meta-analysis attached. And let’s not forget the FDA’s ‘labeling’ which, as we all know, is just a polite suggestion written by lawyers who’ve never seen a patient. The real world doesn’t run on statistical noise - it runs on anecdotes, fear, and the terrifying reality that if you prescribe the wrong thing, someone dies. So yes, I’ll keep avoiding all sulfonamides. Because I’d rather be safe than statistically correct. And yes, I know you’re smarter than me. That doesn’t make your opinion safer.
Ben Harris
So let me get this straight - you’re saying my mom’s 78-year-old aunt who got a rash after sulfa and now can’t take any diuretics is just being paranoid? That’s what you’re saying? That’s not just dangerous - that’s cruel. You think doctors are just lazy? We’ve seen people go into anaphylaxis. We’ve seen skin peel off. You don’t get to dismiss that because your rash was ‘mild.’ This isn’t a spreadsheet. It’s human bodies. And you’re treating it like a math problem. I’m not impressed.
Rick Kimberly
Thank you for the comprehensive and meticulously referenced overview. The distinction between antimicrobial and nonantimicrobial sulfonamides is critically underappreciated in clinical practice. I have personally observed the consequences of mislabeled allergies in outpatient settings - particularly among elderly patients with polypharmacy. The SULF-RISK tool appears promising, and I intend to integrate its principles into our clinic’s allergy review protocol. I would welcome access to the validated algorithm or accompanying clinical decision support guidelines for implementation. This is precisely the kind of evidence-driven refinement that modern medicine requires.