Central Sensitization: Understanding Chronic Pain and How Medications Help
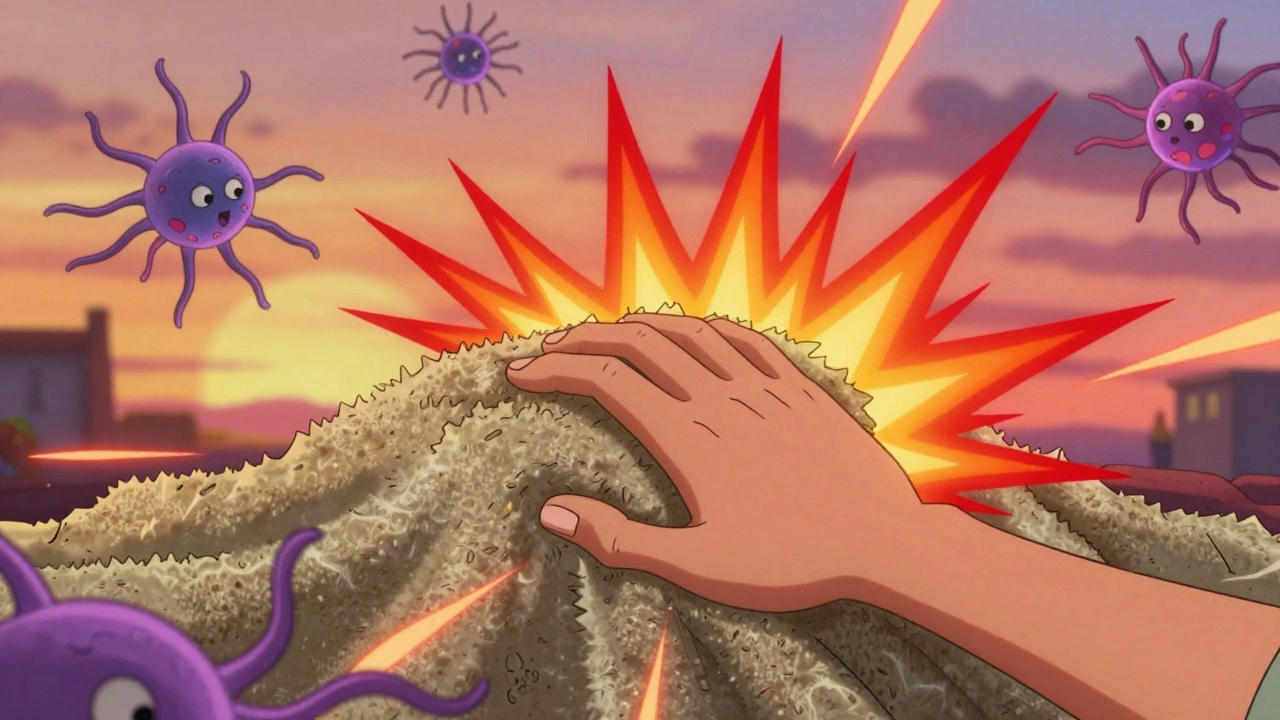
When pain sticks around long after an injury heals, it’s not always because the damage is still there. It might be central sensitization, a condition where the nervous system becomes overly responsive to pain signals, turning normal sensations into intense discomfort. Also known as neurogenic pain amplification, it’s behind many cases of chronic pain that don’t respond to standard treatments. This isn’t just "being sensitive"—it’s a real change in how the brain and spinal cord process pain. Think of it like a thermostat stuck on high: even a warm room feels scorching.
Central sensitization often follows injuries, surgeries, or illnesses like fibromyalgia, complex regional pain syndrome, or even long-term back problems. It’s not rare—studies show up to 25% of people with chronic pain have signs of it. And it’s not just about the spine or nerves. The brain itself rewires over time, becoming more reactive. That’s why some people feel pain from light touches, cold air, or even stress. It’s not in their head—it’s in their nervous system. This is why drugs like gabapentin, pregabalin, or certain antidepressants are often prescribed: they don’t just mask pain, they calm the overactive signals. These medications target the nervous system’s hypersensitivity, not just the site of the original injury.
What makes central sensitization tricky is that it doesn’t show up on X-rays or MRIs. Doctors diagnose it by pattern: widespread pain, sensitivity to touch, fatigue, sleep issues, and no clear physical cause. That’s why so many patients get dismissed—or worse, told it’s "all in their head." But it’s real, and it’s treatable. The good news? You’re not alone. Many people with this condition find relief through a mix of medication, physical therapy, and lifestyle changes. The posts below cover exactly that: how drugs like gabapentinoids work, why some pain meds fail, how hydration and sleep affect nerve sensitivity, and what to ask your doctor when standard treatments don’t help. You’ll find real-world advice on managing symptoms, avoiding dangerous drug combinations, and finding treatments that actually match what’s going on inside your nervous system.