Osteoporosis Inflammation: Causes, Risks, and Treatment Options
When working with osteoporosis inflammation, a condition where bone loss and chronic inflammatory activity intersect, weakening the skeleton and raising fracture risk. Also known as inflammatory osteoporosis, it links immune signaling to bone remodeling processes. This overlap means that osteoporosis inflammation isn’t just about calcium; it’s about the whole immune‑bone connection. People often notice the problem after a minor fall reveals a fracture that wouldn’t happen in healthy bone. Lab tests may show elevated C‑reactive protein alongside low T‑score, pointing to both inflammation and decreased mineral content. Understanding that the two processes feed each other is the first step toward a plan that tackles the root cause rather than just the symptoms.
Key Players Behind the Bone‑Inflammation Cycle
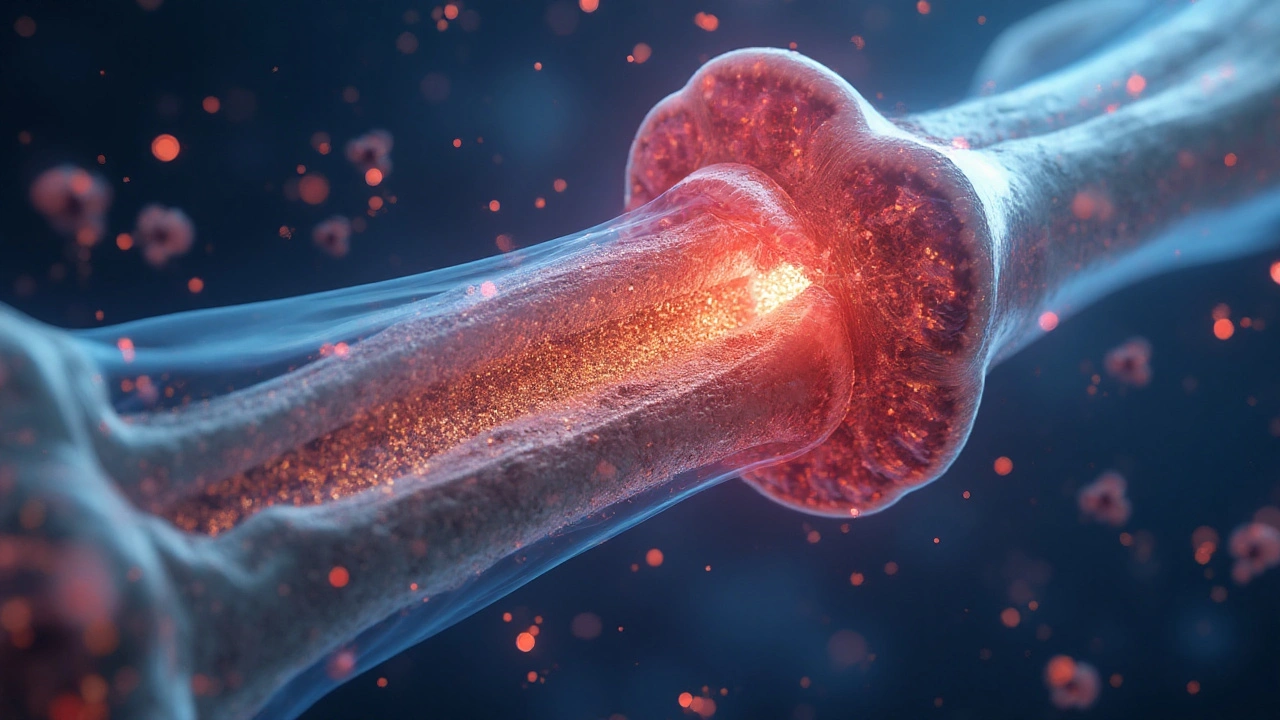
The first factor is bone density, the amount of mineral packed into bone tissue that determines strength. Low bone density often signals that osteoclasts, cells that break down bone tissue during normal turnover are overactive. Those cells become hyper‑responsive when cytokines, signaling proteins such as TNF‑α and IL‑6 that drive inflammation flood the bone micro‑environment. The semantic triple here is clear: Osteoporosis inflammation requires cytokine activity; cytokines stimulate osteoclasts; osteoclasts reduce bone density. Other contributors include hormonal shifts—post‑menopausal estrogen loss removes a natural brake on osteoclasts—and lifestyle factors like smoking, which amplifies cytokine release. Even gut health matters; dysbiosis can increase systemic inflammation, indirectly nudging bone loss. By mapping these relationships you can see why a single lifestyle tweak rarely solves the problem; you need a multi‑front approach.
Therapeutic options aim to break this loop. bisphosphonates, drugs that inhibit osteoclast‑mediated bone resorption are the most prescribed class for slowing loss, and studies show they can reduce fracture rates by up to 40 % in high‑risk patients. Adequate vitamin D, essential for calcium absorption and bone mineralization and calcium intake support the skeleton while anti‑inflammatory strategies—such as omega‑3 fatty acids, regular moderate exercise, or targeted biologic agents that block specific cytokines—lower the inflammatory push on osteoclasts. Emerging research points to selective estrogen receptor modulators (SERMs) and newer anti‑RANKL antibodies as additional tools that directly dampen the bone‑immune feedback. Lifestyle tweaks like resistance training improve bone formation by stimulating osteoblasts, the cells that build bone, creating a healthier balance. Understanding that osteoporosis inflammation encompasses bone density loss, cytokine signaling, and cellular turnover helps you choose a plan that tackles both sides of the equation. Below you’ll find articles that dive deeper into each element, from the science of cytokines to practical dosing tips for bisphosphonates, so you can build a personalized, evidence‑based strategy.