Immunosuppressants: What They Are, How They Work, and What You Need to Know
When your immune system turns against your own body—attacking healthy tissues in conditions like lupus, rheumatoid arthritis, or Crohn’s disease—it needs to be calmed down. That’s where immunosuppressants, medications that reduce the activity of the immune system to prevent damage to healthy tissues. Also known as anti-rejection drugs, they’re essential for people who’ve had organ transplants and those fighting autoimmune disorders. These aren’t antibiotics or painkillers. They don’t kill germs or ease discomfort. They silence your body’s defense system, and that’s both powerful and dangerous.
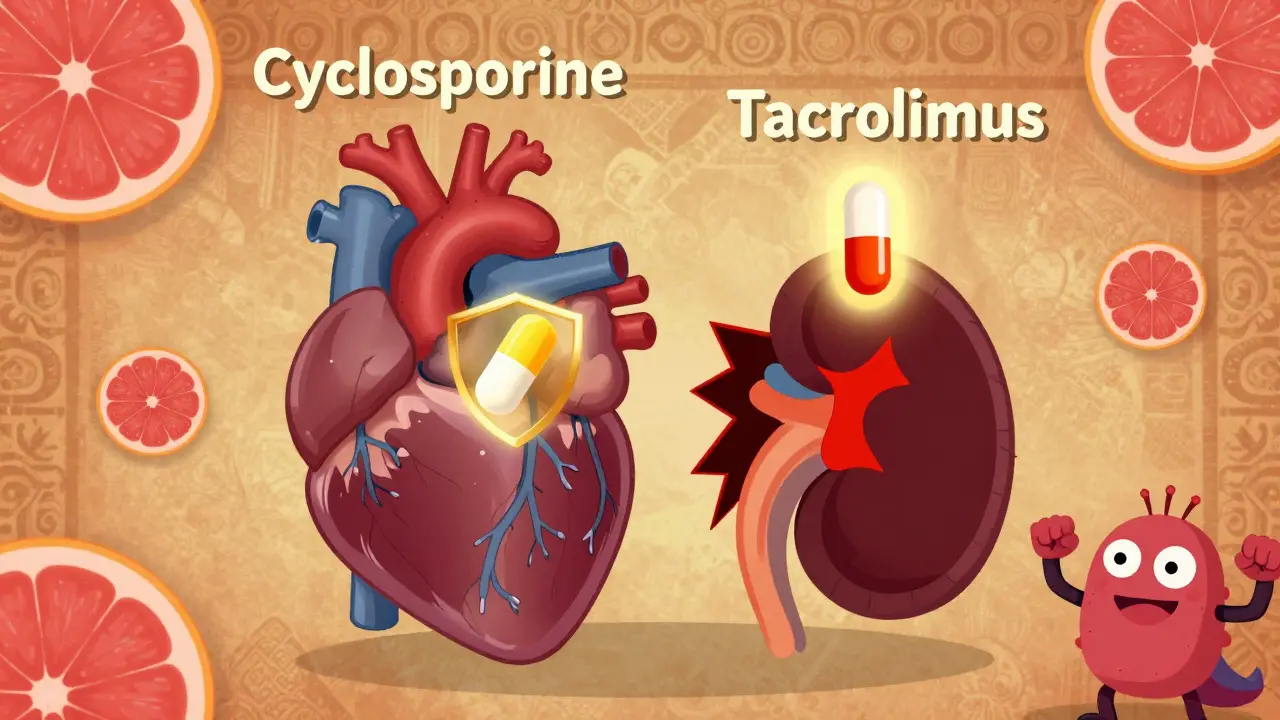
Immunosuppressants are used in three main scenarios: after a kidney, liver, or heart transplant to stop the body from rejecting the new organ; to treat severe autoimmune diseases where the immune system attacks joints, skin, or intestines; and in rare cases for severe allergic or inflammatory conditions. Common types include cyclosporine, a drug that blocks T-cell activation and is often used in transplant patients, tacrolimus, a stronger alternative to cyclosporine with similar goals but different side effects, and azathioprine, an older but still widely used drug that slows immune cell production. Each works differently, but all carry the same core risk: making you more vulnerable to infections, cancers, and other complications.
People on these drugs need regular blood tests to monitor kidney function, liver health, and white blood cell counts. They’re often advised to avoid raw meat, unpasteurized dairy, and crowded places during flu season. Even a minor cold can turn serious. Some users report tremors, high blood pressure, or swollen gums—side effects that aren’t talked about enough. And while these medications can be life-saving, they’re not a one-size-fits-all solution. What works for one transplant patient might cause severe side effects in another with lupus.
The posts you’ll find here cover real-world issues people face with these drugs: how to avoid infections while on long-term therapy, why lab monitoring is non-negotiable, how to handle missed doses, and what happens when they stop working. You’ll also see how they interact with other medications—like opioids or antibiotics—and why mixing them can be risky. There’s no sugarcoating here. These drugs save lives, but they demand constant attention. If you or someone you care about is taking them, this collection gives you the practical, no-fluff facts you need to stay safe and informed.